Stopping Gout Together › Forums › Help My Gout! The Gout Forum › First severe gout flare after bodybuilding
- This topic has 7 replies, 6 voices, and was last updated 4 years ago by
nobody.
-
AuthorPosts
-
-
November 19, 2017 at 12:28 am #5935
 SmithParticipant
SmithParticipant
Should have wrote an outline for this… TL;DR at bottom if this is too much to read.
Gout became severe about 5-6 days after I quit drinking. Never really drank much beer, but was a very heavy drinker. I fear it was a fasting and feasting flare because I couldn’t eat much while drinking that much and when I started eating again it was literally pounds of roast, brisket, lunch meats. The flare was terrible, got better briefly with the first medicine, but has come back. Kind of feels like it is headed to the other big toe, but no swelling and much stiffness yet. I have also had terrible flatulence… MORE INFORMATION:
I weigh around 300lbs but am right at about 200lb of muscle mass based on DEXA scan and electric analyzer at complete nutrition. So ~33-34% bf is high. I generally lift weights 4-6 times a week when I am not doing my manual labor job.
I have taken almost all high purine foods out of my diet but the damn information online is so conflicting. Eggs and whey protein are my main source of protein right now. I had probably 6-8oz of salmon last night. Rice, spinach, banana peppers go with those meals. Whey protein goes into a blueberry, raspberry, blackberry, and today added dark sweet cherries to the smooth of approximately 1.5-2 cups of fruit.
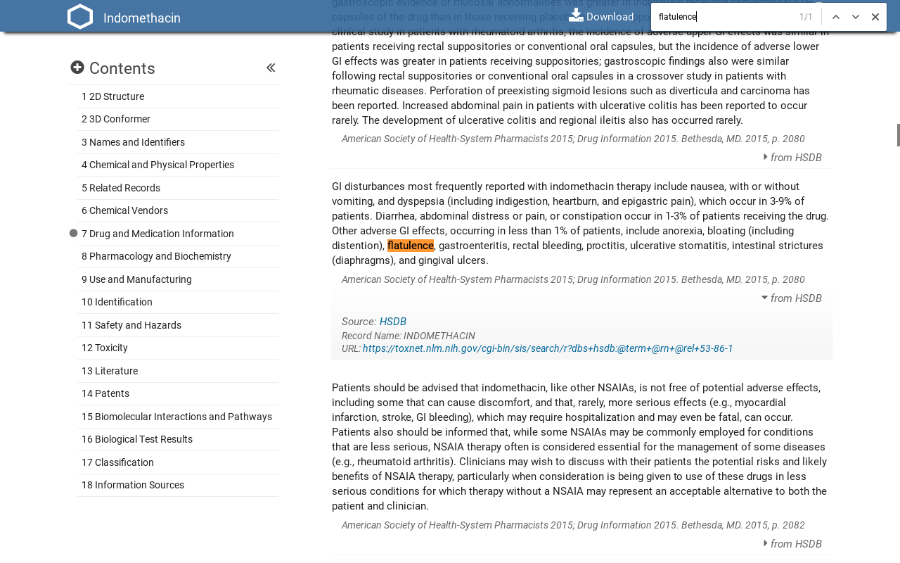
Podiatrist put me Indomethacin which gave me terrible acid reflux. I can keep it under control with a large meal. I was using these for a while and haven’t got through the whole bottle but the side effects are not so great. So, he also gave me methylprednisolone which I’m feeling much better with both of these. Not sure if the Indomethacin or gout has given terrible gas but it is pretty constant.
HOWEVER, I fear these medicines are masking symptoms and not doing anything for treatment which is not going to be okay because I work in steel toe boots, running, jumping, and lifting all day. I haven’t been to work in over 2 weeks now because of this hell.
Sorry for the long post.
——
TL;DR: Quit drinking, fast/feast potential reaction, overweight, changed diet completely, on short-term fixes from meds so I can get back to work, but want this to never come back – need to know what to do… What are my best courses of actions to make sure this flare stops quick, I keep it at bay for at least 6 weeks, and lifestyle changes necessary to never see this hell again.
Why does bodybuilding cause gout?
-
November 19, 2017 at 7:40 am #5936
 Keith TaylorParticipant
Keith TaylorParticipantWhenever gout is linked to food, it’s all about what you ate last year. Not last week. (For the experts I know that’s a simplification. But I’m starting with the obvious until we have more relevant information. )
So the most likely explanation is your parent’s combined genes make you susceptible to gout. Then bodybuilding amplifies the problem. Think of it like driving very fast cars when your parents gave you short sight. Because you could stop driving. But you would still risk other hazards. So the sensible option is specs. Or other eye correction.
The sensible option with gout is allopurinol. Or other uric acid control.
Windocin (!) for Gout?
-
November 19, 2017 at 4:10 pm #5943
nobody
ParticipantYes, “these medicines are masking symptoms”.
Unfortunately allopurinol is not a quick fix. It’s quicker and more effective than lifestyle modifications so that’s not an argument against allpurinol.
I only bring up the bad news because I’m seeing red flags in Smith’s post:
-podiatrist
-“terrible acid reflux”
-“he also gave me methylprednisolone”
-no mention of a PPI
The side effects of these drugs sometimes get worse over time… much, much worse. And chances are this isn’t the last time Smith will need to take anti-inflammatories.
I obviously can’t know what’s going on in Smith’s stomach (doctors need to push a camera down your throat in order to assess that) but prolonged use of that drug combination is known to involve a risk of stomach damage which a drug class called PPI can at least delay if not completely prevent. And once stomach damage becomes obvious, it’s too late to prevent it.
If you think gout on anti-inflammatories is hell, try gout when you can’t take anti-inflammatories anymore because of stomach damage!
So I would recommend seeing a doctor who understands GI side effects better than the average podiatrist. Maybe that podiatrist is awesome and understands well things outside of their specialty. But if not… -
June 2, 2018 at 12:10 pm #7131
Donnavan
GuestI have been suffering from Gout for the past 5 years now. I have recently managed to get the gout attacks under control as my doctor has prescribed that I take one puricos tablet a day.
Since then I have been very active in the gym and started weightlifting and bodybuilding.As I understand the effects of puricose, is that it removes excess uric acid from the blood and therefore minimizes the probability of a gout attack. My question is – will the puricos negate my bodybuilding targets due to reduced intake of protein. Protein is necessary for muscle growth. if this is the situation, then is there an acceptable protein supplement that can be recommended that will not aggravate gout?
Thanks.
-
June 2, 2018 at 10:40 pm #7133
nobody
ParticipantSo far as I know, the tablet doesn’t affect protein intake.
Eggs for instance contain plenty of proteins. Whether it would be a good idea for you to eat lots of eggs depends on other aspects of your health. Provided your puricos dose is sufficient, you could eat meat as well. Regular foods are safer than processed supplements but you can always get your blood tested to see what the supplements you take are doing to your body.
You should probably get tested anyway if you’ve recently beeen exercising or bodybuilding a lot more than you used to. Depending on your test results, changing your puricos dose might be prudent. -
June 28, 2018 at 1:10 pm #7220
 Fred DeerParticipant
Fred DeerParticipantHave you tried Diclofenac? It worked for me. After 3 months of agony my first gout attack in my ankle cleared in 48 hrs. It was never diagnosed as gout as I never had a toe attack first so they told me it was a sprain. A wise nurse prescribed it to me.
I then did have a toe attack but all other attacks were in my knee and ankles so it took about 5 attacks till I recognised it felt the same and then ablood test confirmed it.
I only need take a pill when I feel a gout attack coming. It then subsides in a few hours but at most 24hrs. Sometime I need to take one or 2 follow up pills a few hours apart.
Before Diclofenac my gout attack would last a week or 2. I ended up walking on crutches diagnosed with arthritis.
My sign of an attack coming is waking up with a join pain somewhere in my ankle/Knee/toe that appears for no reason. That’s when i reach for it.
Changing my diet and stopping drinking had no effect.
-
March 31, 2019 at 6:41 pm #8851
Cathy Dawson
ParticipantGout and Gastric Reflux
Hi this is Kathy in Colorado. I have had offered on burning feet for about five years. The past year I decided to take more control of my health and lost 25 pounds slowly. Still, the gout pain is getting worse. My uric acid tests at 6.3. I seem to notice that when I even eat fruit now the pain starts immediately. And now I am having other bad symptoms of fatigue, back pain, and a recent blood test showed that I have inflammation going on. Also, a high ferritin level. Iron level is normal though. I am seeing a functional medicine practitioner tomorrow, and I am finally willing to try some meds. But I dread the meds because my liver function is low.
I had hoped I could finally win this battle With diet choices alone. My feet and especially all of my toes burn constantly and now I can’t sleep because of it. Also, I have gastric reflux and overall feel pretty miserable.
Any help or suggestions would be very welcomed. What would be the first line of meds to try that have the least amount of side effects?
-
April 1, 2019 at 1:11 am #8852
nobody
ParticipantI can’t help you with the reflux other than to say that, like gout, it’s sometimes a misdiagnosis. Unless an examination has demonstrated that reflux is indeed the problem, it could be a stomach or gallbladder issue for instance.
Assuming you really are suffering from gout, it sounds like you’ve only had one uric acid test. If so, get it tested again!
You might well be able to win this battle with diet alone in the long run, especially if you count weight loss as part of diet. It would require patience however. Most of the information about gout and diet out there is also quite bad so make sure you aren’t wasting your time by trying to make the wrong changes to your diet.
Meds could be a great help while you are losing weight and ajusting your diet. The important thing, considering your liver issue and the 6.3 uric acid test (I assume you’re not misreading 0.63 mmol/l as 6.3 mg/dl which would completely change the picture), is to stick to very small doses of allopurinol (and if your doctor wants to give you febuxostat which is also known as Uloric, the dose you ought to try first should be no higher than 10mg which might well be a problem depending on where you live). You could also try completely different drugs or indeed foods known to lower uric acid but the nice thing about allopurinol and febuxostat is that they work well enough that a very small dose could well be sufficient. Even with common foods known to lower uric acid, you’d have to consume so much that it might be hard on your liver for all I know.
Possibly you might also get results by lowering your ferritin. See if that might have something to do with the fatigue you’re experiencing. But you should also find a way to lower your uric acid.So far I have only been talking about drugs acting on uric acid but there are also drugs you could take to alleviate your symptoms. Unfortunately the drugs most people take for gout symptoms often cause liver function problems and you often need large doses for gout. If you can’t use regular anti-inflammatories because of your liver (if you haven’t tested what that does to your liver, I would strongly recommend against testing a regular anti-inflammatory at the same time as a drug which lowers uric acid), one thing you could do is to take a painkiller to help you sleep (keeping in mind you need to avoid anything containing paracetamol/acetaminophen).
If your doctor suggests colchicine instead of an anti-inflammatory, be aware that is also known to trigger liver function issues. They’d have to look into less common gout drugs if they want to suppress inflammation without endangering your liver.
-
-
AuthorPosts
The forum ‘Help My Gout! The Gout Forum’ is closed to new topics and replies.