Stopping Gout Together › Forums › Help My Gout! The Gout Forum › Painful feet! Is it Gouty Arthritis?
Tagged: Forum for Arthritis Sufferers, Forum for Gout Foodies, Forum for Gout Patients, Lingering Gout Forum, Most Helpful Gout Forum, Should I Walk with Gout Forum
- This topic has 38 replies, 10 voices, and was last updated 4 years, 7 months ago by
vigrom.
-
AuthorPosts
-
-
August 19, 2016 at 3:28 pm #1624
 Irma ReitzParticipant
Irma ReitzParticipant
Painful feet and gout.
I’m not sure if I have gout but I know I cannot continue in pain any longer. I have painful feet – it feels like I’ve got broken glass inside my feet – its the tops of my feet and toes as well as my ankles that hurt when I walk or stand. My feet also hurt at night in bed if one foot is on top of the other. X-rays reveal arthritis and blood test shows slightly elevated Uric acid levels. GP says I should try to reduce foods with purines as he does not want to prescribe any Meds to reduce the Uric acid at this stage. He also told me to lose weight(I’m overweight). He has prescribed a natural product called Piascledine (soya and Avocado extract)for arthritis, which I have been taking for 5 weeks with no improvement. I take anti-inflammatories twice daily, but nothing seems to help. I discovered this site and thought that perhaps I have gout or gouty arthritis and was hoping that I could find a way to ease the constant pain. I would appreciate any input and advise.
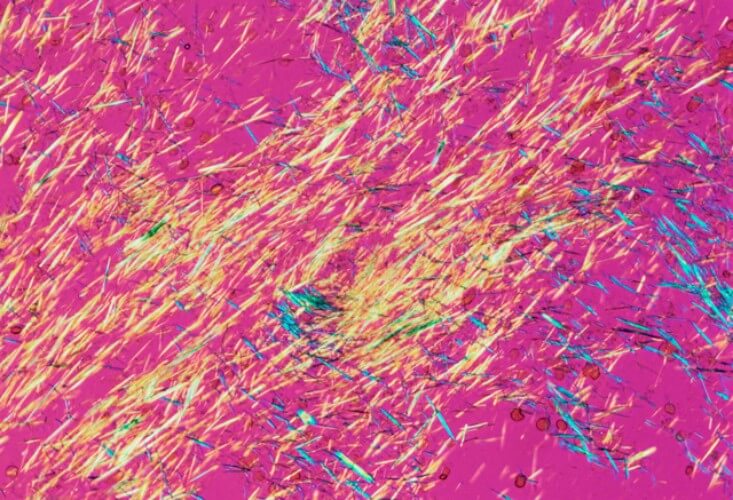
[image added by admin]

Does gout make your feet sore like running a marathon?
-
August 19, 2016 at 7:37 pm #1630
 Keith TaylorParticipant
Keith TaylorParticipant“slightly elevated Uric acid levels” doesn’t give me enough information to help. I need the exact number. I’ve heard doctors call 8mg/dL “slightly elevated”. It makes me mad. Anything above 7 is dangerous, and needs urgent treatment.
I hate the idea of withholding treatment because you’re overweight. That’s just nonsense. I’m still overweight. But I found it much harder to lose weight before I got my gout under control. Some doctors don’t understand.
I understand your situation completely. I can help you through this. But I need very specific information.
As well as your exact uric acid numbers, I need to know exactly what meds you are taking with their daily doses.
Help me to help you, Irma. Gimme the numbers! I’m a data geek ❗ 🙂
-
August 19, 2016 at 8:08 pm #1631
 Keith TaylorParticipant
Keith TaylorParticipantI just spotted you said “gout or gouty arthritis”, Irma.
They are the same thing. Gout is a form of arthritis. Gouty Arthritis is the long name for gout, often used by the medical profession.
-
August 21, 2016 at 1:53 pm #1661
 Irma ReitzParticipant
Irma ReitzParticipantI have been reading your advise and recommendations of finding a rheumatologist and am trying to find one in my area. I live in a small town in the Western Cape, South Africa and have managed to locate one in a larger town 110 kilometers away. So I intend to collect my X-rays and blood tests to show the rheumatologist once I can get to see him. Is there anything specific I should ask when I see him? I am quite excited as it may be an end to this constant pain in my feet and ankles. I have started at the gym – Stationary bike and weights 3x weekly.
I will give you the Uric acid numbers when I get the tests back.
I take the following supplements and medication:-
Meds :-
Premarin o.625mg (conjugated oestrogen) 1 X daily evenings
Coxflam 7.5mg (meloxicam) 2 X daily – morning and evening
Piascledin?? 1 tablet daily mornings (soya & avocado extract for relief of osteoarthritis)
Paracetamol 500 with codeine. 1 tablet nightly (sometimes another during the night if in pain.Supplements :-
Omega 3 – 500mg daily mornings
Turmeric Curcumin – 1000mg daily mornings
D3 – 400iu daily morning
Probiotic – 1 daily mornings
Vitamin C – 500mg daily mornings
Co-Enzyme Q10 – 50 mg 1 daily mornings
Supercal bone food – calcium/magnesium/zinc/manganese/boron/vit d3 1 daily evenings
Chelates Zinc – 22mg 1 daily eveningsI have on occasion used colchicine for a few days, which has helped when I’ve been really sore.
Thank you once again for your help. I am so grateful to have found your site. Keeping fingers crossed.
Irma
-
August 23, 2016 at 2:19 am #1689
 Keith TaylorParticipant
Keith TaylorParticipantAnd, thanks for reminding me that I used to wonder about the difference between gout and gouty arthritis. It prompted me to include an explanation in Gouty Arthritis Sufferer Or Not?
In fact, that could be written for you Irma, as it deals with the common situation of the uncertain gout sufferer. That article is the starting point in this situation. I’m wondering if I’ve included all the different types, though. As an uncertain gout sufferer, do you identify yourself as
one of the following three types:
1. You have a doctor’s diagnosis of gout, but you doubt it is true.
2. You think you have gout, but your doctor doesn’t agree.
3. You think you have gout, but you will not consult a doctor.Is there a fourth type – “doctor not sure?”
As a starting point, I’m only interested in people identifying themselves as members of GoutPal’s Arthritis Sufferers Group. One of my important pieces of advice, depending on the answers to my 2 questions, is “consult a rheumatologist”.
I’m pleased to see you are doing that, Irma. Would you indulge me, and give me your opinions on my article?
-
-
August 23, 2016 at 12:21 pm #1704
 Irma ReitzParticipant
Irma ReitzParticipantHello Keith.
Thank you so much for all you do for us. I have read your very informative article on ‘Gouty Arthritis Sufferer on Not’. I am in the second category ‘I Think I have gout but my doc does not agree’. I am encouraged by your article because even if it turns out that I do not have gout, there is still a whole lot of help there to manage pain.
I collected my blood tests results and am not too sure on how to read them. I have used your Uric acid calculator and I think my level is 6.5.
My serum analysis is as follows:- please will you help me to discipher the numbers.
S-urate 0.38 H 0.15-0.36mmol/LI forgot to mention that I have Vogel Multiforce alkaline powder first thing every morning in an attempt to become less acidic as I thought it was acidity that was causing the pain and also have a teaspoon of ginger powder in hot water as my early morning drink. Ugh! I’ll try most things to try to alleviate or control my discomfort.
Re weights – I thought I would try out for Tokyo Olympics!…
-
August 23, 2016 at 9:02 pm #1705
 Irma ReitzParticipant
Irma ReitzParticipantuh oh! Big error! I tried to upload a copy of my blood tests in the wrong place. Sorry! I created a support ticket and have given you extra work. Silly me. My apologies
-
August 26, 2016 at 4:04 am #1711
 Keith TaylorParticipant
Keith TaylorParticipantHi Irma,
Please don’t worry about the blood tests photo you sent. That’s exactly the right thing to do. It’s very useful to see the actual result. It means I can see exactly what you see.
You’re right about the numbers. You are just below 6.5 mg/dL. I’m guessing the H means High. This is significant. Many doctors will not treat below 7mg/dL (0.40 mmol/L). I find that very odd. The correct target for treatment in most patients is below 5mg/dL (below 0.30mmo/L).
Returning to your meds:
– Premarin (conjugated oestrogen) is associated with reduced uric acid in women.
– Coxflam/Mobic (meloxicam) is associated with slightly reduced uric acid in rats.
– Piascledine – no information relating to uric acid found.
– Paracetamol/acetaminophen – the jury is out! Unlikely to have any effect at normal dose.
– Omega 3 – new research suggests this is excellent for reducing frequency of gout attacks. I’m investigating further.
– Turmeric Curcumin – Again, I’m investigating some new research which adds more evidence to show how curcumin from turmeric helps reduce uric acid.
– Vitamin D – recent research suggests a genetic influence and a link that is “clinically very small”. To be honest, “Potential causal associations between vitamin D and uric acid: Bidirectional mediation analysis” is very difficult for me to understand. I don’t think it’s significant: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4586492/
– Probiotic – too little evidence. 1 study shows insignificant increase in uric acid. Another shows insignificant decrease.
– Vitamin C – Vitamin C lowers uric acid. But note that other studies have failed to find significant benefits in gout patients.
– Co-Enzyme Q10 – little evidence. I only found one study, and that found no link between Co-Enzyme Q10 and uric acid.
Nothing on the other 2.I’ll talk about meds in your new thread.
Supplements are a very personal topic. As far as uric acid is concerned, many effects depend on the individual. I think the best approach is to have a healthy diet, then use supplements for specific vitamins and minerals where necessary.
I’m particularly forthright on that topic when it comes to alkalizing. It goes against everything I believe healthy to take alkalizing supplements. pH balance should come from natural food and drink. But, that’s just my opinion of course! Alkaline diet is good for gout.
-
September 16, 2018 at 4:20 am #7743
vigrom
GuestHello there!
First off, millions of thanks for your very helpful newsletter and for the tremendous effort you are putting into it!
Second, have you ever considered a connection between gout and vitamin D? If per chance not yet, this URL might be a good starting point (I am not affiliated with that website in whichever way) – [link to spurious site removed]
Thanks again and kind regards,
Viktor
[Posted via replying to email update service. But note that you should not reply to email updates. Because there is no way to post these automatically to the forum. In this case, I could not work out what you were replying to. So I posted it to the only recent topic that mentions Vitamin D with respect to gout]
-
-
August 28, 2016 at 8:30 pm #1740
 Irma ReitzParticipant
Irma ReitzParticipantWow Keith! You are so right – I should not be taking alkalising supplements, but I am feeling desperate as I am in pain and I thought that it might help. Your article on alkaline diet is really interesting. There is so much info that I am struggling to absorb it all and can’t remember what have just read, so I keep re-reading. Maybe some will stick! I am trying to plan a diet to help my gout and arthritis. I need to loose weight which I know will help, but at this stage all I’m trying to do is get my pain under control. I think that I normally have a healthy diet, although I do go off the rails now and again. I can’t get to see the rheumatologist for 3 weeks, which seems like such a long way off. Today was particularly bad, as I had a bad night and am very tearful and depressed. I am encouraged when I browse this site, because it gives me hope. Thank you again.
-
August 29, 2016 at 1:42 am #1741
 Carolyn PoulterParticipant
Carolyn PoulterParticipantHi Irma, I have nothing factual to add to Keith’s advice, he has done the research and thanks to this site I have researched more and more and am beginning to find answers to my particular situation.
What Keith gives us is access to answers to our many questions and, perhaps most of all, the reassurance that we are all different when it comes to gout and how to overcome stereotypical thinking by our doctors.
Any old how, as they say on corny US sit-coms, I feel your pain. I know just how you feel at least for me, the pain over-rides all sensible or ludicrous thought. On a scale on 1 to 10 with 10 being childbirth – and in my day no epidurals unless you pre-booked them so for me it was ‘Like or lump it girl’. When I had my third son he was over 9 pounds I did grab hubby’s chest hairs through the gown and said ‘This is all your effing fault!’ and he did get a vasectomy a couple of weeks later but I am digressing, yet again – on that scale 1-10 I would say gout is a firm 11 or 12.
It is just horrible and until you have experienced it first hand, you just can’t understand how painful it is. Nor can you convey that to other people like doctors. If they’ve never had it, they will never understand.
Hang in there, keep asking questions and don’t take their (doctors) answer as gospel. Doctors, GP’s, are great, they work hard, but they are basically clearing houses. They identify and send you to a specialist, or they identify and say ‘it will go away’.
Please keep sharing your experiences. It might not match or ‘fix’ my problem but everything I learn about the condition helps and I fell more in control because of that. Hope I am making sense here. Just took my daily Allopurinol tablet and that always sends me a bit squiffy.
-
August 29, 2016 at 8:34 am #1742
 Irma ReitzParticipant
Irma ReitzParticipantHey Carolyn. Thanks for that. Somehow it helps knowing someone understands. I love reading your posts – so amusing – makes me giggle. Pain is just normal today not like the past 3 days so it is manageable. I’m never sure whether to take the colchine (just in case) or just to stick to my regular anti inflammatories and painkillers and only take the colchicine when I’m going through the roof. Going to omit it and see how it goes.
I can’t wait to start on a programme to remove the Uric acid crystals, so waiting impatiently to see the rheumatologist and work with him. Have a great day. -
September 1, 2016 at 2:51 pm #1762
 Irma ReitzParticipant
Irma ReitzParticipantOh no! Pain back with a vengeance. Started taking the colchicine again yesterday 1 milligram daily, plus a new anti-inflammatory ‘Vimovo’ – ingredients 500mg naproxen 20mg esomeprazole, twice daily. Apparently this med has built in stomach protection. These were prescribed for my husband when he had a knee replacement and so I just had a repeat script filled for myself, after discussing this with the pharmacist. I had been taking an over-the-counter anti-inflammatory but it’s not strong enough. I know! I know! I shouldn’t do this but I’m not coping with the pain. I also take paracetamol with codeine as needed. I just can’t understand why the pain is so out of control as the moment. My feet have always been painful but now the pain on right foot, the top inside is unbearable. I’m going on holiday for 2 weeks and seeing rheumatologist when I get back. I can’t wait to start get a diagnosis and to start treatment to reduce the Uric acid.
-
September 2, 2016 at 2:15 pm #1768
 Keith TaylorParticipant
Keith TaylorParticipantIrma, your last response is very close to what I was about to suggest.
Gout pain lingers, for most people I encounter in this forum, for one simple reason. They don’t take pain meds at gout strength. OTC doses are fine for those days when the gout pain isn’t too bad. For a full blown attack, it has to be a medically prescribed gout strength dose.
The other thing is that a combination is almost always required.
Colchicine slows inflammation but does nothing for immediate pain. It should be taken daily as a preventative (usually at the start of uric acid treatment), or as required. If taken as required, you have to take it at the first sign of an attack.
Anti-inflammatories are good for reducing inflammation, and this reduces pain.
Paracetamol blocks any residual pain.
Always check with your doctor, or a pharmacist, that combinations are safe. They will also advise what is the safe maximum for bad gout days.
The only other thing is to keep mobile. When pain hits, you often want to curl up in bed. But, the pain goes quicker, in my experience, with gentle exercise. Therefore, once the meds have made pain bearable, go for a walk, or a swim. This is vital advice for holiday enjoyment. Once you take control of gout pain, the tears pass. Then, you can focus on controlling uric acid, and stay gout free forever.
-
September 3, 2016 at 4:51 am #1772
 Keith TaylorParticipant
Keith TaylorParticipantIn a hurry, I said “The only other thing is to keep mobile.”
That’s not strictly true.
The 3-pronged attack on pain is vital: Block Inflammation (colchicine). Reduce Inflammation (Anti-Inflammatory). Block Pain (Paracetamol/Acetaminophen, etc, etc). And, it’s vital that the package is dosed to gout strength and safety checked by a qualified doctor or pharmacist.
If that is done right, mobility should not be an issue. You might have some residual stiffness for the first 20-50 yards. But, that should pass. If not, do not push too hard – residual pain after your 3-pronged combination is an indication the package isn’t right.
The most important “other thing” is personalization.
I do not know of alternatives to colchicine, so leave it out if you can’t tolerate it. Some people opt for a steroid shot instead of colchicine/anti-inflammatory combo. Not for me, but it’s your choice. There are hundreds of anti-inflammatories and pain blockers. If your current choice isn’t working for you, ask your doctor for something else.
-
-
September 2, 2016 at 3:37 pm #1769
 Carolyn PoulterParticipant
Carolyn PoulterParticipantIrma, I am so sorry to hear the pain is back.
I have been on Allapurinol now for about 6 weeks and once the huge flare up had finally started to wane I have been trying to cut back on the pain-killers. Paracetomol with Codeine is prescription only here and I didn’t bother to ask the doctor for that. He did give me seven days of an anti-inflammatory, no idea if it helped or not, the pain was so bad I would have been happy being hit over the head with a mallet and knocked out so I fully understand you being a bit naughty and taking your husband’s pills.
BUT this Tuesday I woke up and said to hubby ‘I can feel my feet and they don’t hurt!’ Then I got up to go to the loo and ouch ouch ouch ouch, but not as bad as before. Wednesday I finally got outside, albeit with a walking stick, sighed because of the drought my garden is toast and came back indoors. Yesterday I walked down to the mail box, 500 yard driveway and very steep and only twinged a bit. Today it seems even better, just the odd twinge in my feet and base of my thumbs. Slow release Ibuprofen keeps it to a dull burn.
I am going to ask the doctor to keep me on the Allopurinol, he might resist, but I am going to try to stand my ground. Here we have to pay the full price of drugs, it’s not like the UK prescription charge thing, but Alan’s insurance is covering 75% of it at the moment. I am not very good at standing up for myself with authority figures like doctors but I will try. You should see me going through customs, I always feel like my face looks guilty and I’m not!
I do hope you feel better soon. I have been looking into rapid weight loss/crash diets/anorexia and gout. I also had a dip back into anorexia way back in my late 20’s and had gall bladder problems. Gall bladder removed when I was 30. In a mental hospital which my husband just loves to tell people about – long story I won’t bore you with here, maybe on an off-topic discussion.
I am also trying to be more mobile as Keith advises. I am sure he is right though it is oh so tempting to just curl up and whimper. Ballet dancing is probably now in my past but then, even after 13 years of classes when I was in school I was always more of a Fantasia Hippo than Swan Lake. Instead I am planning on walking more and more each day. Alan is off work next week and I have booked a couple f nights away – hotel, swimming pool, hot tub, nice meals and not quite real champagne, and if the weather is good, a trip on the Thousand Island Cruise – which is basically us with a bunch of others on a boat, drinking wine while we look at very posh houses on private islands which I am sure the rich people hate as we float by waving at them! Heh.
Get well soon Irma!
-
September 12, 2016 at 6:58 pm #1941
Gout Patient
ParticipantHi Irma,
I’m also a SA member so feel free to pm me.
First of all switch docters – I’ve battled for 30 years with this deadful disease and the main cause was that docters think they are Gods gift to Mankind.
You can take 300mg Puricos twice per day combined with a 5mg Colchicine each time and 2 tablets Panamor Diclofinic to help break the pain initially
Ideally you must start with 100mg for week one, then 200mg for week two and three and then 300mg from week four.
This is necessary to get your body used to it. Believe me it is necessary.
I’ve been taking 600mg Puricos for going four months and it is only getting to work now.I’m also seeing some tofu shrinking for the first time ever.
You can also get a cortisone injection which will give immediate relief – but it is poison.
The Banting diet is excellent for losing weight – follow the Low carbs high fat on facebook. Personally I’ve lost 15 kg in 4 months with no effort.
And yes, it is advisable to gettting a bloodtest done on your kidneys and liverfunctions. It can always be used as the base case when evaluating results. Prolonged use of Diclofinic will lead to a loss of kidney function. 70% in my case! Don’t let this happen to you.-
September 13, 2016 at 6:23 am #1944
 Keith TaylorParticipant
Keith TaylorParticipantHi Johan,
It’s great to have another new member from South Africa. You’ve made some great points.
It’s fantastic that you’re seeing positive results with Puricos. Am I right in thinking that Puricos is 100% allopurinol? It’s good to see your gradual introduction: 100mg rising by 100mg increments. To make this a perfect introduction to allopurinol, dose should be guided by uric acid blood test results. The only reason for taking allopurinol is to get uric acid to your target uric acid level. That means you have to have a target that is safe, and suits your personal situation. It’s usually below 5mg/dL. But, every Gout Patient should have their own target. And, Target Uric Acid should be reviewed annually.
We don’t know anything about your uric acid levels Johan, so I can’t comment on whether 600mg is the right dose for you. If tophi are shrinking, it seems right without considering anything else. But, if the aim is tophi reduction, then I’d usually recommend maximum allopurinol for at least six months. Everyone is different.
Finally, on allopurinol dosing, it’s usually better to review and change dose every 2 weeks. That’s because it takes 2 weeks for allopurinol to stabilize. 1 week is probably OK if you have tophi. I say that because tophi sufferers should be aiming low as possible, so weekly blood tests are really a safety check rather than a dosing guide. That implies you are doing blood tests right, and getting liver and kidney function tests with your uric acid tests.
I agree with your recommendation against long term use of diclofenac, but that’s the first time I’ve seen a warning for kidney damage. I thought the biggest threat from long term NSAIDs was heart attacks. Anyway, it’s best to limit NSAID use for a few weeks while uric acid lowering does it’s job. I also agree that steroids are a very bad thing, but I respect other views if cortisone is a necessary last resort. My beef with steroid use is when they are used as a lazy first option before trying other effective remedies.
Finally, Johan, I’m intrigued by your Bantang diet. I’ve never heard of it before. Please would you be kind enough to start a new topic about Bantang diet and gout? I’d love to know what Bantang diet is, and how is it beneficial to gout sufferers?
-
-
September 13, 2016 at 1:43 pm #1970
 Irma ReitzParticipant
Irma ReitzParticipantThanks for your input Johan and your clarification Keith. I’m on holiday in the Kruger Game Park at present with limited internet coverage so a quick reply. I’m just trying to get through the holiday and to cope with the pain so am living on paracetamol with codeine, colchine and NSAIDs for the next 10 days. Long stretches sitting in the car plus safaris vehicles over rough roads have taken their toll on my back and I can hardly put any weight on my right hip😢. It is really spoiling what should be a wonderful experience getting back to nature and seeing all the wild animals and birds. My appointment with the rheumalogist should hopefully provide some answers.
-
September 13, 2016 at 1:47 pm #1971
 Irma ReitzParticipant
Irma ReitzParticipantOh by the way Keith. The Banting diet is similar to The Atkins Diet.
-
October 30, 2016 at 8:34 am #2206
Gout Patient
ParticipantOriginal post by Johan
Midfoot Gout Problems
So People,
Had to visit a top foot specialist in South Africa this week.
Reason was the severe pain inside the top of my right midfoot.
Now, this has been ongoing for most of my adult life – am turning 62 soon.
Even this extremely experienced gentleman did not have an explanation of why the cartilage in this area has disappeared or why there are holes in my cartilage.
All I can say is that I had suffered from gout in this foot in all its forms for years.
Fourteen years ago(cannot believe it was that long) I was infected with an Aureus virus from a doctor’s injection for the start of a gout attack. Fortunately, I survived that incident. But it destroyed a lot of the tissue in the area and caused damage to the cartilages.
So now I am destined for foot surgery with a painful recovery period of at least 6 months. It is also a very expensive procedure. Don’t even mention the word uncomfortable. Just Google midfoot surgery on Youtube. You’ll probably faint.
The reason why I mention all of this is to warn you against the probable long-term consequences of gout attacks which our doctors conveniently forget to inform us off.
ANY infection of ANY sort between two joints must be considered the same as you would view a heart attack.
Please don’t play around with uric acid levels and such. Later in your life, you just might regret the decisions you made when you were young.Regards All,
Johan -
September 1, 2017 at 8:05 am #5564
 Keith TaylorParticipant
Keith TaylorParticipantNo More Gout!
That’s the last time I use the G-Word – at least for today. Because the only way to stop it forever is to change the way we look at it.
Urate Crystal Arthritis is so easy to cure, you don’t even need help from a website. 😉
Here is a new way to stop gout. Much more than a name change. Urate Crystal Arthritis is easy to control. See how to control uric acid arthritis today.
-
December 30, 2017 at 11:39 pm #6301
d q
ParticipantSlightly interesting website – opinions anybody?
@nobody, @keith – just a little read for us;I’m generally not a believer of all the homeopathy treatments when it comes to gout except the benefits of cherries however I stumbled on this and this. Both sites seem pretty new on the internet. Interesting information up there but not exceptionally new to us.
Now most of the information on those sites we already know however my emphasis is more on the second link here. Aside of he’s attempt to convince us to purchase etc. and I’m not actually sure it will work in my case since I believe I have secondary gout (rapid red cell turnover releasing UA into the blood) so purines don’t really count but have any of you tried to heavily alkalise your diet to see if much lower UA can be achieved? Is this actually feasible?
Another thing I wanted to discuss was he’s opinion on how Febuxostat and Allopurinol work. He makes it clear that these are very damaging, @keith I was wondering if you had any information from your library about long term use of these drugs (Febuxostat being relatively new)?
p.s. He’s statement about Lemon and Vinegar being acidic and dangerous however seems wrong as I understand these turn Alkaline upon entering and metabolising in the body? I have emailed him about this and am still waiting for he’s response.
And… On a more social note, Happy New Year 🙂
-
December 31, 2017 at 10:03 am #6304
nobody
ParticipantHomeopathy is something else.
I don’t understand your blood condition but I would imagine that it causes higher UA through purines (just not dietary purines).
I’m not sure what “heavily alkalise your diet” means but I haven’t noticed any effect on SUA from the amount of magnesium, calcium and so forth in my diet. Then again, because of the noise and the sparse data any effect would have to be quite large to get noticed.
I have no reason to doubt it has an effect but I would assume the effect varies quite a bit depending on how much UA someone’s body produces, kidney function and so forth.Unsurprisingly, some of the information on these pages is wrong or presented in a misleading way. For all I know, most of it might be accurate but I certainly wouldn’t bet on that. The anti-pharma verbiage and the fact that a product is being sold are quite the red flags.
Do you have any reason to trust these sites? Is there any particular morcel you found intriguing or illuminating? -
January 1, 2018 at 5:40 pm #6306
d q
ParticipantWhilst not Homeopathy in the respect of the required components, he is suggesting not to use pharmaceuticals and instead buy this “Calkaline” alternative.
Yes, my gout is due to an increased rate of red cell production. The technicalities are out of the scope of this thread.
I have no particular reason to trust this site neither do I suggest trusting these sites especially since it promotes the selling of a product (or an e.book on other sites) but it seems one can Alkalise their diet at home eliminating the need to purchase he’s product. I too question some of the information on the site and even emailed him but the interest (more so the curiosity) was to know if anyone has actually tried substituting water with alkalised water on a long term basis and seen progress in a way that can be a substitute to common UA lowering drugs.
The very reason I raised this post here was for us to question the possibility.
Has anyone got research articles or documentation as to whenever its been tried?
Is the replacement Alkaline water approach (not baking soda) safe / feasible? -
January 4, 2018 at 10:58 pm #6312
d q
Participant@anybody – have you tried replacing water with alkaline water and pressing on with it for a period of time?
-
January 5, 2018 at 3:40 pm #6313
 Jean ClyneParticipant
Jean ClyneParticipantYou may know that lemons while considered acidic act as alkaline in the body, so drinking water with lemon is good because it acts alkaline. Another way to easily drink alkaline water is to cut up 1 lemon, 1/2 cucumber, 1/4 peeled ginger root and 1/2 cup fresh mint. Put all in jug of water overnight and drink glass in morning on empty stomach, also take during the day. There are many different versions of this, also lists of alkaline high foods that are good to consume. I am currently giving this a try, sounds healthy and can’t hurt body or wallet.
-
January 6, 2018 at 3:38 pm #6315
d q
Participant@jean – this is exactly what I am thinking of trying but on an intense scale.
More out of curiosity and interest rather then treatment to start with.Do you have your uric acid blood levels before you started your trial..?
cheers
-
January 7, 2018 at 4:53 pm #6317
 Jean ClyneParticipant
Jean ClyneParticipantMy ua blood levels are always in normal range but did go down after 6 mos on allopurinol. It really caused a lot of side effects for me so went off it abt. 4 mos ago, have since been going alkaline and 300 to 400 mls black cherry juice which has allowed me to be symptom free. Coincidence? Don’t know, time will tell. I should get another ua blood test in a couple more months, will be interesting to see what that shows. My other option is uloric but don’t want to go there unless I really have to, which may be necessary at a later date.
-
January 8, 2018 at 11:25 pm #6318
d q
ParticipantInteresting you say that, I was on Allopurinol for about 6 months and although I am not certain, it caused me bad haematological side effects (doctors are not convinced of this however) They believe it could have been because of the inflammation I had at the time. What about yours?
In any case I am on Febuxostat (Uloric) now and things seem to be stable. I’ve been on the drug since the middle of November and going up slowly (breaking pills into half and further into half, etc.).
It would be great to see what your latest UA blood test will show and if the Alkaline approach works.
p.s. How are you achieving your alkaline approach..?
-
January 9, 2018 at 4:36 pm #6319
 Jean ClyneParticipant
Jean ClyneParticipantI am totally vegetarian, eating lots of fruits and vegetables lean towards a more alkaline diet it seems. I drink water that has lemon, ginger, cucumber and mint in it from one of those jugs that has a container in the middle for extras that the water filters through, in addition to probably 300 plus mls of cherry juice a day. There is lots of info out there on alkaline foods versus acidic. I wonder if the bad side effects I got from the allopurinol were because my ua levels were in normal range? Does poor circulation in hands and feet contribute to the gout? I had Achilles tendon thickening that went away totally after 6 mos. on allopurinol,, was that related to gout? Glad to hear uloric is working better for you, sounds like it has a lot fewer side effects. I wish my Dr. would refer me to a rheumatologist who would maybe have some answers to my questions.
-
January 21, 2018 at 2:28 pm #6358
d q
ParticipantHi Jean, sorry for the delayed answer.
I am not too sure what you mean by ‘Bad side effects you got from Allopurinol were because your levels were in the normal range’. Why would you take Allopurinol if you were in the normal range to start with?
In answer to your questions;
Although I am not certain but poor circulation wouldn’t really help as the lower temperatures (less blood to the area) would generally increase the likeliness of Uric Acid crystallising in that area.
Generally speaking long term hyperuricemia will also cause a build up of uric acid in muscle tissue too. So yes, you could have had a build up of uric acid in your muscles which can lead to pain in those areas too. The thickening could have been a result of joint effusion in which your body was in a chronic low grade inflammation state.
Again I am no doctor and base my comments on experiences and tests.
Although high Uric Acid doesn’t always lead to gout I would certainly recommend you keep an eye out on your levels even if you decide not to take any long term medications. I am not trying to deter you from a drug-free approach but it could just be that you are symptom free because Allopurinol did a good job of clearing out lot’s of long term build up over the 6 months you were on it.
Uloric seems to be working but things are a little tricky at the moment with reductions not being entirely fair to dose increases. Let’s see how things develop over the next few weeks.
-
January 23, 2018 at 4:45 am #6361
 Jean ClyneParticipant
Jean ClyneParticipantMy doc said that normal uric acid levels were fairly common in some patients that still had gout. What I wonder is because my uric acid levels were in a normal range, did trying to lower them further with allopurinol cause more side effects than most others that have high ua levels to begin with. The allopurinol did eliminate my gout symptoms and eliminated the Achilles tendon thickening that I did not realize were likely from uric acid deposits. After having those for years, why would they then disappear?At present as I previously said, cherry, alkaline diet and increased dairy consumption have kept the previous gout symptoms away. How long this will work for, I have no idea but so far so good for the past 4 months.Will get uric acid levels tested again soon.
-
January 27, 2018 at 6:33 pm #6462
 Keith TaylorParticipant
Keith TaylorParticipantI’ve got very mixed emotions on this one @d_q
Because, on one hand, Mr. Hemen Ee from Malaysia seems a nice guy who is just trying to raise some money to support his family.
But, on the other hand, he’s suggesting poisoning us with ionic calcium as a great way to find gout freedom. No ingredients, no safe dosing advice, no suggestion of testing for blood ionic calcium levels or testing urine pH.
So, it’s a dodgy, potentially dangerous, sales pitch for something that is unlikely to work. Also, it begs the question I always ask regarding similar baking soda claims. Why would you risk dangerous chemical imbalance in your body when you fairly easily achieve alkaline urine through healthy diet changes.
Then my emotions go into overdrive, as I realize how little work I’m doing on Foodary and EFSEP. Because they are my projects to encourage healthy eating. Usually, alkaline-diet based, but with easy stages to help the transition from unhealthy Western Diet.
Also, I realize that my reliance on advertising and commission revenue is compromising my integrity. Because I cannot vet all robotically-served adverts to ensure they are not making misleading claims like Mr. Ee’s websites.
So, I’d better commit to moving personal support to a paid service, so that I can remove adverts and commission links. Also, I’ll commit to introducing my Gout Foundation Diet plan. But instead of wasting time working out ways to provide it for free, I will charge for it. Though I hope I can offer generous discounts to you and the other lovely people who commit their time to making my forum better.
And… On a more social note, Happy New Year 🙂
I don’t think it’s too late to return the compliment, @d_q.
So I hope 2018 brings you everything you wish for. And a special thank you for making me think about important things.
-
January 27, 2018 at 6:42 pm #6466
 Keith TaylorParticipant
Keith TaylorParticipant -
January 27, 2018 at 7:23 pm #6472
nobody
ParticipantOpinions are a dime a dozen and all but I don’t see your integrity being compromised by random ads. Random ads are everywhere.
I’d be more wary about the integrity of someone who sells premium content frankly. Not as such of course… it would depend on the premium content, how it’s pushed and so forth.
-
-
May 5, 2018 at 4:15 pm #6987
 DaveParticipant
DaveParticipantBall of foot gout pain and swelling
Been controlling my gout daily with 300 mg allopurinol, cherry complex and uric acid support supplements along with major diet changes. I’ve been monitoring my UA weekly with a monitor for the past four months and I’m averaging 3.9 mg/dl.
All has been going well until a few days ago when the ball of my right foot has all the signs and symptoms of a acute gout attack. With my UA levels controlled and low, I’m thinking this may be the crystals breaking down from the metatarsal joints.
Right now I’m treating with prednisone to relieve the inflammation, OTC pain control and increasing my H2O intake.
This may be totally unrelated to UA and something along the lines of metatarsalsia which I’ll have to get a consult from a podiatrist.
My inquire is to see if anyone else has experienced this same condition and what if any the findings were. Additionally I’m wanting to reduce the dosage of the allopurinol and at some point not take it anymore. This begs the question: how does one know when this is?
Thank you.
David
-
May 5, 2018 at 4:47 pm #6988
nobody
ParticipantHi!
You should definitely not quit allopurinol while you are experiencing this type of symptom, unless you’ve been able to rule out gout as a cause. It often takes more than 4 months to get rid of crystals and you want to get rid of all your crystals before attempting to live without allo.
Since you test around 3.9 though, you could try to lower your dose a bit. Or you could stick to 300mg if you have no compelling reason to lower your dose as larger doses than necessary may help keep attacks short. I can’t guess what an appropriate dose would be based on the information above and my guesses wouldn’t be worth much anyway. You’ll just have to experiment!
Ultimately it is your symptoms which will tell you what dose is appropriate and whether you can go without allo. But it can take years for your body to give you definitve feedback. In the meantime you can use UA blood tests as a rough guide: while you are still experiencing gout-like symptoms, 5.0 or less is best whereas once have been free from gout for 6 months of more, as much as 6.0 might be fine. -
May 8, 2018 at 11:14 am #6998
 Steve BatesonParticipant
Steve BatesonParticipantHi Dave,
Ball of foot is certainly where it gets me the worst. Last spring it started as a lump on top of the foot and after some massage seemed to morph through and I had a large swelling underfoot for about three weeks. Can be either foot, often starts in one then travels to the other.It was that that finally (after 9 years of random symptoms) got me a referral to a Rheumatologist who quickly determined gout was the cause.
Ultrasound showed Synovial thickening, MTP joint effusion and small erosion.
Its not confirmed, but I believe this has led to splaying of the gap between 2nd and 3rd toes that has been growing for some years.At the moment I’m on 2oomg allopurinol daily (6 months now) and Colchicine as required. Also Vit C, H2o and cherry extract. Urate is coming down so hope to reduce the drugs in a bit.
Colchicine, Naproxen and co codamol are always close at hand.
Steve
-
-
-
AuthorPosts
The forum ‘Help My Gout! The Gout Forum’ is closed to new topics and replies.