Stopping Gout Together › Forums › Help My Gout! The Gout Forum › What questions should we ask the gout specialist?
Tagged: Adenuric/Febuxostat/Uloric Forum Topics, Allopurinol Problems Solved, Forum for Gout Patients
- This topic has 11 replies, 3 voices, and was last updated 4 years, 4 months ago by
 Sian James.
Sian James.
-
AuthorPosts
-
-
July 21, 2018 at 3:26 pm #7423
 Sian JamesParticipant
Sian JamesParticipant
Hi Guys,
I would very much value your feedback on what questions we should be asking the rheumatologist we are seeing privately on Tuesday – having finally given up on trying to get timely responses in the NHS.
I first posted on the forum a few months ago, and following the excellent advice given, my husband’s gout attacks have improved – but not stopped. Even after two years of treatment, lifestyle change and dietary change, he’s still getting regular flares every three weeks or so, which he dials back with NSAIDS and colchicine. He’s sixty three, and his level of physical activity is constrained by the inflammatory responses he gets to sustained exercise. O
His history is of ten years worth of getting fobbed off and misdiagnosed, and finally diagnosed with gout in 2016. At that point, his plasma urate level was around 650 umol/L (range 200 – 430). He was was titrated up to 400 mg allopurinol daily, but the attacks worsened, as did his overall levels of energy etc. We did both understand the phenomenon of de-bulking. He was switched to 80 mg febuxostat daily a few months later, and finally the dose of febuxostat was raised to 120 mg daily. His most recent urate level, this January, was 149 umol/L.
He has complicating factors – his GFR tends to be around 60, and his mother and aunt both had rheumatoid arthritis, and ultimately died of complications arising from it. He is negative for RA antibodies, but an MRI last November showed inflammatory changed in the for of increased signal in the anteriovertebral body corners. The consultant also talked about inflammatory spondyloarthropathy with peripheral arthritis. Since that MRI, we have been unable to get an appointment – despite the promise that we’d have one by April. Hence the private visit. The Rheumatology department were also talking about starting DMARD’s – eek…
His father has gout and low GFR, but it is well-controlled by allopurinol.
Having read papers questioning the safety profile of febuxostat, particularly in terms of cardiac health, I’m concerned that he was switched from allopurinol before it had a chance to demonstrate its efficacy in the long-term. His GFR has gone down with the raised dose of febuxostat.
He’s been very good at weight lose and dietary change. But we’re both worried about the effects of a poorly-controlled inflammatory cascades over the long term.
Any thoughts on what you would be asking at this point, in terms of further investigations or medication reviews?
Thank you in advance for your responses.
-
July 21, 2018 at 10:17 pm #7424
nobody
ParticipantIt seems like the NHS failed you pretty badly.
With regard to the medication review, the febuxostat dose your husband has been taking is obvisouly excessive. Keeping this up would be reckless. If you want to frame that in the form of questions, you could ask:
-what purpose could this dose possibly achieve?
-did the medical guidelines change while we weren’t looking or something?
More to the point, I guess you could also ask whether it would be advisable to switch back to allopurinol before seeing how your husband fares on a reasonable febuxostat dose such as 40mg.But the main difficulty here is completely different, namely determing what disease your husband might have besides gout. And I’m effectively clueless about spondyloarthropathy and all that. So I don’t know what questions to ask.
The only way I might be able to help you is by telling you what information I’d bring to the appointment:
-a clear and precise description of what you call flares: location, duration and so forth (if you had pictures, that’d be great)
-a precise timeline of the treatment: you want a list of blood test results to establish for how many months the treatment has been successful in reducing uric acid to the recommended values
-a short report about what colchicine does and doesn’t do for your husband’s flares
-and of course all the relevant medical imagery if the specialist doesn’t have it already
All I can say is that, on the basis of the information you’ve given, it’s too early to rule out residual gout as the cause of some of your husband’s symtoms. After many years without treatment, getting rid of gout sometimes takes even longer. I should warn you some doctors are unaware of that fact. That said, the spine thing is so far as I know not typical of gout. -
July 22, 2018 at 7:37 am #7425
 Keith TaylorParticipant
Keith TaylorParticipantHi Sian,
That’s a great response from Nobody and here are my immediate thoughts.
I can see from your first message (Guidance on febuxostat, colchicine, and NSAIDs) that your husband’s uric acid levels have been 250-300 since around December 2017. Unusually, your rheumatologist’s advice at that time was to aggressively increase febuxostat dose to 120mg. So that resulted in uric acid of 149 μmol/L in January this year.
Personally, I’m a fan of such an aggressive approach to reduce the time for uric acid debulking. But that has to be something that is agreed by doctor and patient. Because a thorough risk assessment of high-dose uric acid treatment is important. Also, we’re all concerned about the long-term effects of febuxostat compared to allopurinol. So, it is important to leave the consultation with enough information for you and your husband to be happy that he is getting the right uric acid treatment at the right dose.
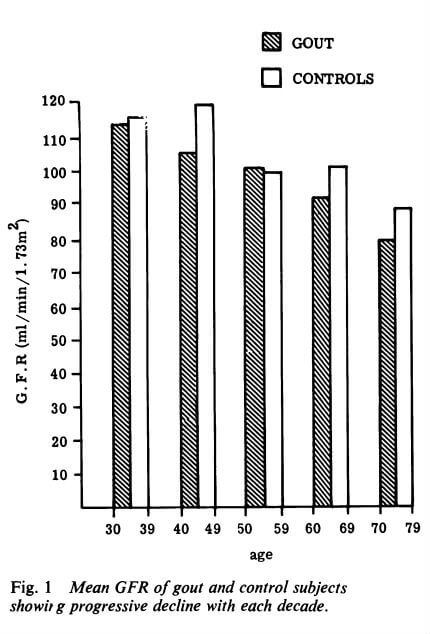
With respect to GFR, I’ve learned that it tends to decrease with age and with gout. But studies indicate that both allopurinol and febuxostat tend to raise GFR. So I’d ask your new rheumatologist if she/he knows of any evidence to show which is best. I’m aware that other factors influence GFR so there might not be a definitive answer.
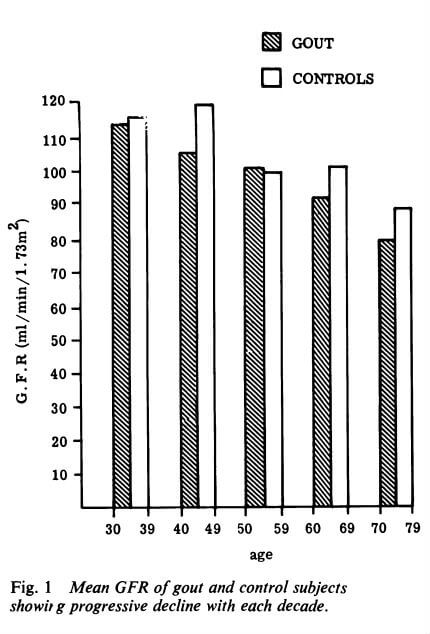
Is low GFR caused by gout, age, or something else?
Unfortunately, none of us can assess the length of time it takes for all old crystals to dissolve. So, as Nobody says, “it’s too early to rule out residual gout as the cause of some of your husband’s symptoms”. However, there is a faint hope that your new rheumy knows where you can get access to a DECT scan for gout management. If so, please tell! Because that’s the Holy Grail for assessing how uric acid treatment is really progressing.
-
July 22, 2018 at 1:00 pm #7435
 Sian JamesParticipant
Sian JamesParticipantThank you Nobody and Keith, those are such helpful answers, filled with great directions that I wouldn’t have otherwise have thought of pursuing. My husband has asked me to pass on his gratitude for your kindness.
I’ll let you know how we get on.
-
July 22, 2018 at 3:04 pm #7437
 Sian JamesParticipant
Sian JamesParticipantmy draft questions, in case they are of help to anyone:
What is the significance of the inflammatory spondyloarthropathy referred to the the letter detailing the results of the MR scan? Is that how the scan reads to you?
2. How definitive is the MRI scan is seeing the full extent of gout damage, tophi etc, and being able to delineate that damage from other forms of inflammatory arthritis? Is a DECT scan necessary or helpful?
3. Given the urate level was 149 when last tested in January, is this current 120 mg dose of febuxostat appropriate?
4. Do you share the concerns about febuxostat and its impact on cardiac mortality? We do have concerns around the safety record of febuxostat, and would like to discuss switching back to allopurinol.
3. Does the history indicate a under-excretion of urates or over-production?
4. How much effect can dietary modification have? And is there evidence to support the lowering of purines?
5. We have received conflicting advice on managing acute attacks – could you clarify what you’ve found to be the most effective method?
6. Does it matter that the last urate result we have was 50 below the bottom of the normal range?
7. Given the strong family history on the maternal side of RA, and death via its complications, is there an autoimmune component to the inflammatory processes identified on the scan?
8. The department letter has mentioned DMARDS. Having seen up close some of the very difficult effects of drugs like methotrexate, we don’t want to blindly follow down a path without a rationale being made to us for their likely efficacy, and their limitations.
8. Given the association between AS and cardiac morbidity, and the association between advanced gout and metabolic syndrome, is it prudent to further investigate cardiac health and metabolic parameters?
10. Given the inflammatory effects noted with AS in the prostate, should relevant prostate testing be undertaken?
8. Could current issues with ‘floaters’ in my eyes be linked to uveitis, given its association with AS?
9. Is testing for the HLA B27 antigen necessary?
10. Given the association between gout and sleep apnea, is it possible to do a sleep study? My wife mentions times when I seem to stop breathing.
11. My ferritin levels went extremely high during his regime of interferon alpha/ribavirn for Hepatitis C. Can we retest iron levels and stores to exclude any abnormalities?
12. My wife has a diagnosis of Lyme disease and babesia via respected lab in the US – and is currently doing a herbal regime to combat it. I have been taking prophylatic herbs myself, and also doxyclicine after a recent tick bite. Given Lyme disease can cause erosive arthritis, is it possible to be tested for it via Western Blot, given the unsatisfactory performance of ELISA tests?
13. What is the most kidney-friendly way forward with both gout, and AS, if I have it?
-
November 18, 2018 at 11:58 am #8749
 Sian JamesParticipant
Sian JamesParticipantQuestions for Rheumatologist
Hi Guys,
Wondered if I could call on your experience once more? We are going back to the rheumatologist next week. She previously was hostile to discussion of whether or not febuxostat or allopurinol had a better profile in terms of side-effects.
My husband, with extensive lifestyle and diet change, and meds, seems to finally have his flares under control. He is currently on 80 mg Febuxostat daily (he decided himself to lower the dose from 120 mg), 1 500 mg naproxen and 20 mg omeprazole in tandem with the NSAID. We don’t have recent urate results. But will have after the appointment. This is the first time in a decade his gout has been under control.
My question – is this a time to continue as we are in terms of meds, or to try and lower or alter doses? What questions should we be asking of the consultant at this point?
-
November 18, 2018 at 2:20 pm #8750
nobody
ParticipantAssuming 80mg febuxostat doesn’t result in alarming blood test results or more subjective unbearable side effects I see no reason to change your husband’s dose at this stage. It’s too soon to declare victory over gout even though any reoccurring symptoms ought to be less violent and/or shorter in duration.
Prolonged NSAID use is dangerous however, especially when a PPI such as omeprazole is required.
If it’s at all possible at this stage to dial down the NSAID dose and maybe take it only on the days when inflammation shows up, that’s what I would recommend. If your husband is ever told to abstain from NSAIDs because he took too much in the past (possibly damaging his stomach or what have you), he’ll be in trouble if he gets hit with serious inflammation again. -
November 18, 2018 at 5:50 pm #8751
 Sian JamesParticipant
Sian JamesParticipantThank you very much @nobody, that helps clarify my thinking. Good point on future usage of NSAIDS. I will see if there’s a way of dialling that back, and/or switching to a less potentially damaging med.
Do you have a view re febuxostat re allopurinol and long-term safety? Or am I treading old ground here?
-
November 18, 2018 at 7:39 pm #8752
nobody
ParticipantIn my opinion, febuxostat vs. allopurinol should be a matter of individual reactions to the drugs and individual vulnerabilities.
Febuxostat has often been claimed to be preferable to allopurinol for patients who have kidney disease but I understand some people are arguing against this claim. I don’t have a serious kindney problem and so I know next to nothing about the issue.
Allopurinol is of course better-tested and febuxostat is more dangerous according to some studies but the dosage is a confounding factor. People often compare stronger doses of febuxostat to weaker doses of allopurinol. Also, strong doses of allopurinol (like the one your husband would probably need) aren’t so well-tested. I wish less biased and better designed medical research would have provided us with more conclusive data but here we are…
So assuming your husband is tolerating febuxostat well and you have no particular reason to be concerned about these elusive cardiac side-effects, I wouldn’t pick a fight with your husband’s doctor on this issue, especially at this stage. You’ll have a better picture of your husband’s requirements later on and a moderate allopurinol dose might become a long-term option at that point.I’m afraid effective alternatives to NSAIDs might be even more dangerous in your husband’s case. Hopefully your husband will simply have less need for anti-inflammatories in the future. But let’s see what your doctor (or doctors) think about that…
-
November 18, 2018 at 7:51 pm #8753
 Sian JamesParticipant
Sian JamesParticipantThat is such a helpful response. Thank you so much for taking the time to write it, we are both very grateful for your time and your experience.
Wishing you the best of health,
Sian
-
November 18, 2018 at 8:00 pm #8754
nobody
ParticipantI just edited my previous post, mostly because I thought I needed to clarify “at this stage”.
-
November 23, 2018 at 1:31 pm #8768
 Sian JamesParticipant
Sian JamesParticipantI just wanted to feedback – my husband’s GFR was 46, and his creatinine 136 – the rhemumie said to stop the NSAIDS and PPI immediately, and that he couldnt
use NSAIDS again. He had only been using them during flares – she was the one that told him to go to a daily dose. So, as you so presciently pointed out, that’s another med for inflammation that we can’t have any frequent recourse to.His urate level is now 140 (RR 200 – 400) so she was open to the idea of him reducing his febuxostat to 40 mg by dividing the tablet.
Thanks again,
Sian
-
-
-
AuthorPosts
The forum ‘Help My Gout! The Gout Forum’ is closed to new topics and replies.