Stopping Gout Together › Forums › Help My Gout! The Gout Forum › Why colchicine with Allopurinol and Indomethacin?
Tagged: Allopurinol Problems Solved, Colchicine Combination Questions, Colchicine Problems Solved, Forum for Gout Patients, Starting Allopurinol Forum, Uric Acid Lowering with Gout Pain Relief Questions
- This topic has 32 replies, 10 voices, and was last updated 4 years, 12 months ago by
Mauri.
-
AuthorPosts
-
-
February 9, 2016 at 3:39 am #4907
 Eric BolvinParticipant
Eric BolvinParticipant
Hi; Recently had a gout attack and treated it with Indocin, colchicine, and allopurinol. Am now taking just allopurinol and doing fine. Uric acid is controlled.
Stopped taking colchicine because it wasn’t insured, but am getting some from Canada.
So when should I take colchicine? I know to take Indocin for acute attacks, but what about colchicine?
-
February 9, 2016 at 3:39 am #2756
 Phil HambrookParticipant
Phil HambrookParticipantColchicine – As a course or adhoc?
Hi
I have Suffered with gout for about 5 years no medication taken but since an op to remove my right kidney 9 months ago I have had frequent attacks since, probably due to my eGFR dropping to 40 after my op (its now holding steady at 43). About 5 weeks ago Doctor put me on 0.5mg twice a day colchicine to clear a recent gout attack then after 6 gout free days go onto Allopurinol 100mg per day (forever!).
I am happy to take allopurinol, I have read its kind to the kidney and see it as a possible way out of gout but the colchicine I am a bit worried about. The first time I took colchicine for 3 days, the gout pain disappeared, although foot still red and puffy the pain had gone but I never got the 6 gout free days as gout came back again so had to go back on them again. I then got my 6 gout free days and I have been on allopurinol now for 2 weeks but another gout attack hit several days ago. More colchicine has improved it so stopped taking it but as I write this I feel gout twinging my big toe! so not sure if I should take another colchicine to nip it in the bud.
Any advice? can Colchicine can be taken adhoc on the first signs of a flare, stopping and starting doses, or should it be taken as a block and not stopped until several days after gout pains and swelling has gone. My instincts tell me the second but I don’t want to put any unnecessary strain on my kidney. I am sure I have read colchicine is a poison.
My UA according to the doctor is only slightly raised but they have diagnosed it as gout. I am scheduled for another blood test in 4 weeks to review allopurinol doses, I have no intention of coming off allopurinol now I’m on it!
Regards
Phil.-
February 9, 2016 at 3:39 am #950
Gout Patient
ParticipantSo I finally had my uric acid level tested on February 4/16 and much to my delight I have gone from a level of 416 umol to 249 umol in the course of taking 300 mg daily of allopurinol since November 11/15. As I told my doctor last week what really seems to be keeping me flexible and pain free in this treatment is taking 1.6 mg daily of colchicine. I have in the past few weeks tried to abstain from taking any colchicine and then get a mild flare up, take 2 tablets of colchicine daily again and within a couple of days back to healthy. So my doctor is trying to wean me down on colchicine,which I agree with, I am not a big fan of any long term medication but my question is this, what would be the long term effect of taking daily colchicine anyways? It is an ancient, naturally derived pharmaceutical that has been used since the times of ancient Greek civilization, apparently, so would it be damaging to take a low dosage for the rest of my living days? I understand that it reduces your white blood cell count and not a whole lot is known about it. I am very thankful that I don’t live in the U.S. as what the FDA has allowed to happen to this very effective treatment is criminal, to say the least.
-
February 9, 2016 at 2:24 pm #967
Gout Patient
ParticipantColchicine is not an innocuous medication. It interferes with microtubules involved in cell division. See standard warning below. As to it being ‘natural’…aresenic is natural as well. The ‘natural’ label just means occurring naturally in nature; it does not mean ‘safe’.
WARNING: Colchicine can damage the bone marrow causing severe anemia, low white blood counts, and low platelets. Reduced white blood cell counts may increase the risk of infections. All patients taking colchicine long-term require monitoring of their blood counts.
-
February 9, 2016 at 4:26 pm #970
Gout Patient
ParticipantThanks for that Linda, I suppose I should have asked my doctor the same question. I am trying to reduce my colchicine daily intake to 0.6 mg currently, with such a reduced uric acid level I am not sure as to why I would be suffering any type of flare ups, certainly, however, the duration and intensity of the flare ups is greatly reduced. As I stated before I am not a fan of long term meds of any kind so I am certainly hoping to stop taking colchicine asap.
-
February 16, 2016 at 1:00 pm #979
 Keith TaylorParticipant
Keith TaylorParticipantColchicine Safety
Linda is absolutely right to warn about colchicine safety. It works by poisoning the immune system. The overview of that is, it’s a balance of pain control over toxicity risks. This is common in treatment of many severe pain diseases.I look at it this way:
If colchicine helps you during your uric acid lowering treatment, it’s a good thing. But, I have several caveats:
1. Uric acid lowering should be managed properly to make the period when you get benefits from colchicine as short as possible.
2. Never take more than 2 colchicine in 24 hours.
3. Avoid colchicine if your immune system is compromised. That might mean some other viral or bacterial disease that you are fighting. It also might mean exposure to sick people.
4. Colchicine should be part of a comprehensive pain management package that also reduces inflammation, and blocks residual pain. Without that, patients are tempted to take too much colchicine, which is wrong. It’s wrong because it’s not safe, but also colchicine above 2 per day has little or no effect, other than to poison you.Colchicine during lowering uric acid
Kevin, Great news with your uric acid test results! 🙂
I think it’s important to understand why you take colchicine when you start with allopurinol. Until most of your uric acid burden has reduced, you are at risk of a gout flare. It takes time for old uric acid crystals to dissolve. The way to reduce that time is to go even lower on your uric acid levels, but that’s a different topic.What you should find, is a decreasing need for colchicine. There are different ways to manage that. You could go ‘as required’ now, or reduce to one tablet per day. Whichever you chose, I think it’s best to make a note of your gout symptoms. You can post that here if you like. Or, I’ll set up a personal profile area for you. That gives you historic data to help planning colchicine dose in future. It also focuses the mind. When you reduce dose, or go ‘as required’, it’s important to act fast if you do get signs of a gout flare.
Personally, I reduced my colchicine to zero within a few weeks of starting allopurinol. But, there’s no right or wrong way. Just reduce colchicine at your own pace, Kevin. You can be happy in the knowledge that uric acid is reducing. Any discomfort you get at your uric acid levels is a sign that old crystals are dissolving. It will become less as the days pass.
Thanks for inspiring http://www.goutpal.com/8959/gout-medication-names-colchicine/
-
February 16, 2016 at 5:28 pm #984
Gout Patient
ParticipantThanks Keith very much for the thoughtful reply and subsequent article which directly addresses my issue. Again I am recovering from a mild flare up which I recovered from Feb 13/16 and which initiated on Feb 10 and was focused on my right big toe although it did not seem to really settle into any of the joints there, it almost seemed as if it was really settled on the side tissue of the right big toe if that makes any sense. Leading up to that flare up I was trying to reduce to 1 tablet, 0.6 mg, daily and within 4-5 days of that reduction a flare up. Over the flare up period I was taking 4 tablets daily, unfortunately, which I will abstain from from here on in. Five years previous to that when I first actually started taking colchicine for gout I was told to take a tablet every 2 hours until diarrhea (ugh!) resulted. At those times I can’t begin to estimate what my actual dosage was, only to say it was a lot. In September of 2014 I was told by a pharmacist that advice was no longer valid and only to take 2 tablets upon flare up and one more in 2 hours and no more within 24 hours as it is basically useless beyond that.
From reading your article you have just posted there is possibly one thing that I maybe doing wrong in dosage and that is taking colchicine in the morning as opposed to before bedtime as you recommend. I am going to start today dosing at bedtime and again work towards reducing my colchicine intake, ideally towards zero at some point.
As stated earlier in another post I had my first flare up at the age of 30, so I have suffered with gout for nearly 17 years now and up until very recently had never had a correct diagnosis from any doctor and I have found that the doctors I have had in Canada here don’t seem to be overly knowledgeable on the affliction. Within the three months of taking daily allopurinol I have definitely noticed great improvement and I am thinking that after suffering with gout over that many years without correct treatment my recovery will be a little longer than some. Thanks again for your input Keith, it is greatly appreciated.
-
March 13, 2017 at 4:22 pm #2759
 Keith TaylorParticipant
Keith TaylorParticipantPhil, thanks for taking the time to explain your situation.
I can’t give specific help without a proper history of your uric acid test results. I need dates and numbers. For uric acid results, “slightly raised” is in the same ballpark as “a little bit pregnant”. It tells you which medical condition you have. But it’s meaningless in terms of treatment and care.
Generally, there are two dosing schedules for colchicine. And, anything I say must be cleared with your nephrologist. First, you are right to say colchicine is a poison. It stops your immune cells from replicating, because that is what leads to inflammation. But, it does nothing for existing pain.
So, if you are taking it ad-hoc, take it at the first suggestion of a twinge. But, if the flare has taken hold, you need anti-inflammatories as well. Otherwise, it can take 2-3 days for the existing inflammation to subside naturally.
That’s why, when you start allopurinol, most doctors advise preventative pain relief for up to six months. It has to be managed case-by-case, and depends on your reactions and test results. Personally, I was advised to take colchicine for two months as a preventative, then review. In fact, I was confident enough with my pain control procedure that I changed the colchicine to ad-hoc very quickly. But for anyone not confident, I’d recommend preventative colchicine, if you get no adverse events.
My main worry, from what you’ve said, Phil, is that your colchicine prescriptions haven’t been supported with anything for when you take the colchicine after the flare has started.
I’m sorry it’s not as simple as colchicine as a course, or ad-hoc. I understand that doctors don’t have the time to explain different pain control combinations. But I feel, once you understand how different drugs work on different aspects of gout pain, you can control it better.
I think we might have to go back-and-forth with more bits of information before we can tie things together properly.
To summarize:
1. Your uric acid test result history will give me a better picture of where you stand now.2. Your future uric acid test schedule will give me more confidence that you have an effective uric acid control plan.
3. Your attitude to (and tolerance for) colchicine and anti-inflammatories is important. Colchicine alone is rarely enough to support gout patients during the first six months of uric acid lowering.
-
March 13, 2017 at 4:51 pm #2760
nobody
ParticipantIn addition to what Keith said:
-one advantage that comes with taking colchicine as a course is that it is effective from the very start of a flare (no waiting for you to notice the problem, to take the pill and finally for the pill to work its way into your system).
-if you are taking colchicine ad hoc, discontinuing it too early after a flare (or lowering the dose too quickly) may lead to a comeback or to new flares.
-if you are cleared to take 1.0 mg per day you may want to try to take only 0.5 as a course and the second 0.5 ad hoc.Colchicine is something you will have to experiment with a bit (within individualized guidelines provided by your doctors) for best result with the lowest possible dose.
-
March 13, 2017 at 10:12 pm #2776
 Keith TaylorParticipant
Keith TaylorParticipantColchicine is something you will have to experiment with a bit (within individualized guidelines provided by your doctors) for best result with the lowest possible dose.
That’s very true. In fact, it’s true for all gout pain therapies. Find what works for you!
-
March 13, 2017 at 10:13 pm #2777
 Phil HambrookParticipant
Phil HambrookParticipantThanks Keith and other poster for such detailed replies,
I have asked the doctor for a referral to a Nephrologist on 2 occasions but been told they only deal with CKD stage 4 or 5. Mine is stage 3B but I think I am falling foul of NHS spending cuts. I have attended a Urologist clinic once since my op, I only saw the nurse not the consultant. Only advice I received about gout was not to eat game! I have been told that a urologist consultant is probably not the best to advise about gout anyway, so I am on the verge of paying to privately see a Nephrologist if my gout continues to cause me problems, from what you have said he should fill in the gaps that I have in my gout medication plan.
I will ring my medical centre to see if I can get a historic UA record. I remember a while ago the doctor saying that my blood test did not show gout but that it did not mean I have not got gout.
Thanks again for your advice -
March 13, 2017 at 11:00 pm #2783
 Keith TaylorParticipant
Keith TaylorParticipantSorry, Phil. I didn’t realise you are a fellow Brit. So, I assumed you would have a nephrologist, as I’ve been led to believe that’s common in The States. All I meant was, I’m not a doctor, so you should make sure any pain meds you take are compatible with your surgery.
If there are complications, the gout specialist should be a rheumatologist. But, the only complication here seems to be medical staff who advise about gout. But, they haven’t read the professional gout guidelines that our taxes paid for.
Don’t bother with paying private consultants yet. Send me the train fare from Yorkshire. Then, I can take you step-by-step through the guidelines that frontline medical staff should read. I know we can do it here in the forum. But, I fancy a day out! 🙂
Joking apart (i.e. ignore that last paragraph), we can probably fill in the gaps here, online. Have you ever had any other pain control, besides colchicine?
-
March 14, 2017 at 10:38 pm #2814
 Phil HambrookParticipant
Phil HambrookParticipantWell Keith, previously I have only taken over the counter paracetemol or anadin for the pain, so no real pain control before.
I am pleased with the way the colchicine has dealt with the last few episodes but I seem to have only a short time between those attacks. Last one was last Wednesday for a few days, the colchcine (2 x 0.5mg per day) worked well. The last couple of days though I am feeling twinges in both big toe joints with a bit of a burning sensation but its not making me limp. I am hoping its on its way out…..
-
March 18, 2017 at 7:21 am #2819
 Keith TaylorParticipant
Keith TaylorParticipantPhil, if you are coping OK with just the colchicine, it’s probably best to stick with that. Also, best to talk with your doctor about additional pain relief, if you need it. But, let’s hope you are over the worst.
-
-
January 9, 2017 at 9:20 am #2376
Mauri
ParticipantColchicine and Allopurinol
I have been on allopurinol 300 for a year now, started in January 2016 and have had three blood tests and all indicate my Uric acid is below 5.0. The last reading in December was 4,2. During this year I had a gout flare in June and the doctor said it was due to my body clearing the crystals because of the now low Uric acid and to avoid a new attack he gave me colchicine 0,5 to be taken as a prophylactic for 6 months. I did fine and by December my level was 4,3 and finished using colchicine. It is now January 2017 and yesterday I had a gout attack (as usual on the right toe) and I am taking now Indomethacine and hope to control this attack.
My questions are:
– is it possible that after 1 year on allopurinol 300 and readings below 5 I am still clearing crystals and can still get an attack? How long does this process take?
– should I go back taking colchicine as prophylaxis? I am afraid I could get another attack.
BTW: I am 61, normal weight and walk 5 miles every day and eat sensibly.Any ideas? God bless.
Maurice -
January 9, 2017 at 1:44 pm #2377
 Keith TaylorParticipant
Keith TaylorParticipantHi Maurice,
Thanks for all that information. I know it’s heartbreaking if this happens when you are doing everything right. You are lucky to have a doctor that seems to understand gout well. His explanation is correct. And, I refer to that uric acid crystal clearing process as “urate clearance”. Or, reducing the uric acid burden. But, it can’t answer your “How long does this process take” question.
Truthfully, nobody can. There are too many variables. But, I have made up a ‘rule of thumb’. Like all such rules, it is a little vague. I tell recovering gout patients, like you, to expect urate clearance to take about one month for every year you have had gout. Then, the only truth is “the lower your uric acid, the shorter the period for urate clearance”
Because of that, I personally chose to go for maximum dose allopurinol, in order to minimize the time at risk. My doctor gave me full support in that, but I had to try with 3 others before I found a doctor who understood the biology.
So, using my rule of thumb for your urate clearance period. I’m going to guess your gout started when you were around 30. But, I guess your symptoms started many years later. You started allopurinol in January 2016. But, your uric acid will not have got down to 5 immediately. I’m going to guess April 2016. Therefore, my rule of thumb says, 30 months of urate clearance takes you to October 2017.
Obviously, that’s all speculation. There might be a particularly well-hidden cluster of crystals that trigger a small attack on New Years Day 2018. We just don’t know. As I’ve said, you can reduce the risks of an attack. But, it’s always best to be prepared.
If you are the type of person who listens to your body, you’ll recognize the early twinges of an attack. In that case, there is no need for prophylactic gout pain therapy. That also applies if you are confident that you can control an attack quickly, once it starts.
If not, prophylaxis for a few weeks/months might be the answer. But, you have to weigh up the pros and cons with your doctor. Personally, if I was opting for prophylaxis, I’d also insist on an allopurinol dose increase. That might raise the risk of a flare in the short term. But, it would reduce the period of time that prophylaxis was required.
Again, there are no rules for how long it takes. So, I’m going to make up another rule of thumb, on the spot. If you get uric acid down to 2, change the rule to one week of risk for every year of gout. It’s very hard to be precise, but I hope this explains the controllable elements.
That should give you the information you need, Maurice, to improve your gout treatment plan. But, if you need me to clarify anything before you see your doctor, just ask. In particular, I’ve had to guess at things like current allopurinol dose, uric acid test dates and values, etc.
I’m here to help you make the right choice for you. And, we can discuss it whenever you feel the need.
-
January 11, 2017 at 11:45 am #2384
Mauri
ParticipantKeith: first off let me thank you for a very well explained answer. Makes a lot of sense and you are awfully good at guessing… right on the money.
Let me then pick your brain a bit further: my Uric acid level has been below 4,5 since Feb 2016. A month after starting allopurinol 300 it went from 7,0 to 4,1. So I’ve been clearing crystals for a year now but according to your guesstimates, I could be clearing for 20 months since I have had gout for 20 years now. Therefore I could stay put for 8 more months -in theory- or increase the Allopurinol dose and get faster clearance. I am tempted to use colchicine as prophylactic and up the dose. What would be your dose of choice? 400? 500? Don’t worry, express your thoughts and I will run it by my doctor. This is the only med I take, my health is fine otherwise.
Best regards
Maurice -
January 12, 2017 at 3:49 pm #2386
 Keith TaylorParticipant
Keith TaylorParticipantHey, thanks Maurice. It’s nice to get some positive feedback.
My dose of choice might shock you, but there is logic behind it.
First, I started allopurinol properly with a low dose, and increased gradually. Also, I’m not in one of the racial groups that are advised to take a genetic screening test before allopurinol. I say this, not in answer to you. But, other gout sufferers will read this, who are concerned about allopurinol side-effects. I’m not susceptible to any such side effects. So, I see no limits to allopurinol dose.
In the UK, maximum advised dose is 900mg per day. In the USA, it is 800mg per day. Gout PAtients should note that this is not a medical maximum. Under medical supervision, with appropriate liver and kidney monitoring, a specialist might prescribe higher doses.
In short, my dose of choice is 900mg per day. Then, once visible tophi have disappeared, and pain symptoms have gone for six months, the dose can be lowered. At that stage, you can be almost certain that the uric acid burden has dissolved. So, all you need is an annual check for uric acid, liver function, and kidney function.
Of course, a doctor might feel that there is no reason to go for the maximum dose. In that case, I would ask for evidence that a lower dose is better.
Essentially Maurice, it boils down to what you are most comfortable with. You are clearly on the road to recovery. So, it’s up to you if you want to proceed with caution, or race ahead. Either way, it’s a good place to be, compared to most gout sufferers.
-
January 14, 2017 at 10:23 am #2405
Mauri
ParticipantThanks again Keith. I am totally convinced about your strategy to control gout and clear the crystals.
My take/strategy is this: I will start again the colchicine 0,5 as prophylaxis and after a week or so will up the allopurinol dose from the 300 I take now to maybe not 900 but to 600. In three months I will have a blood test and check UA level; hopefully it will be under 4.0. I will take it from there.
In any case, how do you go about upping the dose from 300 to 600 ? Weekly increases of 100? Incrementally? Or just double it in one go? What is your experience with this? The actual dose of 300 sits very well with me; no side effects whatsoever. And also, should I split the 600 in two takes (breakfast and dinner)?
Thanks again for your efforts in summarizing these matters for us. Great help!
Best regards
Maurice
-
January 14, 2017 at 2:47 pm #2409
 Keith TaylorParticipant
Keith TaylorParticipantMaurice, I can’t tell you how happy I am with your positive tone. I’m looking forward to you posting a message in future that you are free from gout. And, I hope you’ll return to encourage other gout sufferers to follow in your footsteps.
As for the allopurinol dose increase, I went from 300 to 600 to 900. That sequence fits the tablet size. 2 weeks after each dose increase, I had blood tests. Uric acid test confirmed that my uric acid level continued to fall. Kidney function and liver function tests confirmed I had no side effects. Those 3 tests are important for all gout sufferers at least once a year. And, they should be repeated whenever medications are changed. Changes include new medicines, or dose increases.
Any new gout patients reading this should note that my 300mg allopurinol dose was preceded by 100, then 200mg. And, if you are of Han Chinese, Thai, or Korean descent, you should get a genetic screening test before starting allopurinol.
There is no advantage from splitting allopurinol doses during the day. Allopurinol breaks down very quickly in the body to oxipurinol. Both help reduce uric acid production. Oxipurinol stays in the body for up to 2 weeks. The implications of that are:
1) It doesn’t matter too much if you miss one day (but try with all your might not to!).
2) Blood test results need 2 weeks after dose changes for results to be accurate.Good luck Maurice! It sounds like you are well on the way to becoming a Gout Champion. 🙂
-
March 17, 2017 at 8:51 pm #2818
Carroll Lee
ParticipantPre-allopurinol Pain Treatment
Should pain treatment (prednisone/naproxen.etc) be initiated prior to allopurinol treatment or be delayed?
If it is prior, how long before the first dose of allopurinol.(100 mg)?
Have said it before will say it again……..excellent website.
-
March 18, 2017 at 7:45 am #2822
 Keith TaylorParticipant
Keith TaylorParticipantPersonally, I don’t think steroids such as prednisone have a place, but that obviously depends on personal circumstances.
Where pain control is take as a preventative, it is best to start the day before starting allopurinol. But, if pain control is “as required”, then start allopurinol first.
-
-
August 2, 2017 at 11:28 pm #4908
d q
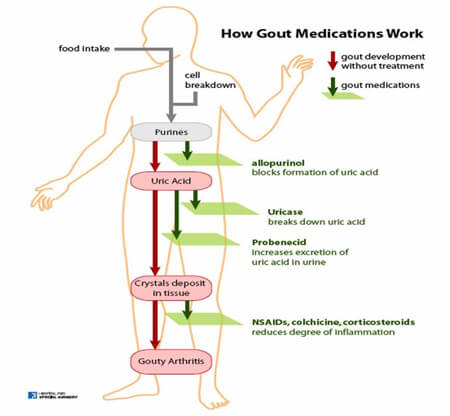
ParticipantColchicine is used for both prophylaxis treatment(preventative) and as an acute attack treatment when you feel a gout attack coming.
Generally speaking, it is administered when starting new uric acid controlling medication such as allopurinol or febuxostat AND when increasing your dose of allopurinol or febuxostat (if required) to prevent attacks whilst those medications begin working and dissolving uric acid crystals or tophi.
It is also taken on the first feeling that a gout attack is about to begin to stop the spread of inflammation and to minimize the length of the attack.
The dosages should be set by your rheumatologist when prescribing it to you. There are generic dosages that you can use but I would recommend you don’t follow them as colchicine can be toxic if administered incorrectly
Take a look at Acute Gout Attack Treatment Plan for a little information.
It is best to seek rheumatologist advice before taking any colchicine.
-
August 3, 2017 at 6:24 pm #4911
nobody
ParticipantOther situations in which you might want to take colchicine while you know you could experience an attack at any time:
Say you’re planning a business trip and you realize that an attack right before or during that trip would be extremely inconvenient. Take colchicine a few days before and during the trip.
Say you’re planning to do something which has triggered attacks before such as a bit of trekking. Take colchicine from the day before to the day after.
You get the idea. Just because you don’t need a prophylactic every day doesn’t mean you never need it.You might also use colchicine if you are afflicted with a persistent attack which indo can’t seem to quell fully or a seemingly unending series of short attacks.
-
August 3, 2017 at 6:57 pm #4913
 Eric BolvinParticipant
Eric BolvinParticipantThanks all!
-
August 5, 2017 at 4:39 am #4927
 Keith TaylorParticipant
Keith TaylorParticipantHi Eric,
Am now taking just allopurinol and doing fine. Uric acid is controlled.
If that’s true, you don’t need colchicine. But is your uric acid below 6 mg/dL (better below 5)? Because 6 is the maximum safe level, and 5 gives a good safety margin.
Finally, if you’ve only just got down to that level, you might still get occasional flares until more old uric acid crystals dissolve. But if Indocin is working OK for you, there’s no need for colchicine.
-
August 22, 2017 at 12:18 am #5387
 urankjj .Participant
urankjj .ParticipantIs colchicine really effective to relieve gout symptoms?
I am assuming that it must be since there are so many people using it. After a quick online Wikipedia (Wiki) inquiry about it though, I must say that I am a bit skeptical about its safety and its necessity for gout treatment.
-
August 24, 2017 at 1:48 pm #5399
d q
ParticipantColchicine for the first time
So the swelling has generally come all the way down but the pain still persists after long walks mainly on the base of my foot and around the top of the toe. As you know I’ve discussed this with two separate rheumatologists and have a professor to see in September. Anyway, I finally decided to give Colchicine a try and took my first 0.5mg tablet this morning to see how my body reacts should I need it.
Anyway, 2 hours into taking it everything seems OK actually. I’m not expecting anything in the way of getting my foot back in shape from the one tablet. It was just to see if I can tolerate the stuff in the event of a flareup prior to starting Febux.
Only side effects I’ve noticed is a dry mouth and throat and an increased urge to drink water, I’ve also noticed a slight headache and a very slight loss of voice. Otherwise things seem OK. I was wondering if these side effects are something you guys experienced the very first time you took Colchicine or every time you took it.
If any side effects did occur during your use, how long did they take to settle down?Thanks guys.
-
August 24, 2017 at 3:37 pm #5402
nobody
ParticipantI don’t recognize the side effects you mention but I might have misattributed “urge to drink water” to stress and/or inflammation when it’s actually a colchicine side effect. Drinking water is healthy anyway.
I might also have shrugged off slight headaches.I’d put the side effects I experienced in two categories:
-weird initial side effects
-dose-dependent gastrointestinal side effects and liver stress
The second category does not go away quickly even if the dose is lowered and and should not be triggered by a single pill. It seems I typically need to take quite a lot of colchicine before such effects become noticable. These are potentially serious side effects and I’ve been told to see them as a hint that I might be taking too much colchicine.
The first category though, I can get that on the first pill especially if I take a full 1.0 mg (I often cut these pills in half and spread the intake over time). In fact, I often get them only on the first pill after a while off colchicine. The most noticeable side effects in that category are itching eyes and feeling like I’ve got a slight fever. But I got other seemingly nonsensical and harmless side effects which go away on their own within hours to a day even in the face of dose increases. -
August 24, 2017 at 5:10 pm #5405
Rebecca Nahid
ParticipantI am one of these weird people that always seems to get Side Effects nobody else gets when I first took Koko Jean I had a big loss of appetite and that’s how I lost a few pounds and yes I was I had a dry mouth and a bit of insomnia I have my body got used to it after a while
-
-
April 23, 2018 at 9:43 am #6949
Mauri
ParticipantHello everyone (specially gout guru Keith):
I wanted to touch base and tell you where I am now. It’s been 16 months (since Jan 17) on allopurinol 600 which has allowed me to keep my UA readings at a steady 3.1 and I have been 10 months without a single flare. Hurray! I believe I have been clearing crystals long enough and I could lower my allopurinol dose, correct? I don’t want to take more than necessary. What should be the goal now? Lower the dose to 100 and keep monitoring UA level and make sure it doesn’t get higher than let’s say 6.5? Is this a sensible approach?? I don’t think I need to stay forever on a 300 dose should I?
Of course whatever I do I will continue to eat sensibly and stay away from seafood, beer, red meat etc. as much as possible.
Any ideas on strategy to use once we believe crystal clearance has been achieved?
God bless
Maurice -
April 23, 2018 at 10:51 am #6950
nobody
ParticipantHi!
The generally recommended maintenance target is 6, not 6.5. After clearing all their crystals, some people are apparently able to substantially exceed that value for months or even years without experiencing gout symptoms but that is obviously risky.
Perhaps you could try taking 200mg (two 100mg pills) for a month or two and see what test results you get on that dose. It may be prudent to lower your dose slowly (or that may be a pointless precaution, I don’t know). -
April 24, 2018 at 10:36 am #6955
Mauri
ParticipantThaks! Will try 200 mg and see where it goes from there..
Best regards
-
-
AuthorPosts
The forum ‘Help My Gout! The Gout Forum’ is closed to new topics and replies.