Stopping Gout Together › Forums › Help My Gout! The Gout Forum › Gout Attack Severity and Duration with Epsom Salt
Tagged: Allopurinol Problems Solved, Forum for Gout Patients, Lingering Gout Forum, Most Helpful Gout Forum, Prednisone For Gout Forum
- This topic has 34 replies, 5 voices, and was last updated 3 years ago by
 Keith Taylor.
Keith Taylor.
-
AuthorPosts
-
-
April 6, 2017 at 9:07 pm #3010
d q
Participant
Hello, good to see these boards have become very active recently. So much information flying about, poor doctors have to deal with our extensive knowledge when they see us now 🙂
One thing I’d like to ask the community is gout flare period and severity.
I started 100 mg of allopurinol in mid December which dropped UA levels from 600 to 555, in mid January my rheumatologist increased this to 200mgs and in mid March UA dropped to 388. He then increased the dose to 300mgs and one week later I got (and still have) a really painful gout flare. Now I’m putting this down to dissolving crystals etc. It’s just that we are in the first week of April and the attack has been going on for 12 days. The pain gets better some days and worse other days but in most cases it’s excruciating whilst walking and at night. I’ve stopped taking Naproxen because it wasn’t helping too much and as far as I know taking it for too long isn’t ideal (10 days +)
I mean if this is what the pain is like now and I assume at least another week for recovery after the pain ‘begins’ to subside!
My question here is how long can attacks take? Has anyone suffered attacks this long?
I’ve got the blood forms to check my UA levels ready and can have them done tomorrow but from what I understand you can’t do a blood test during an attack because the numbers will be wrong / inconsistent. Is this actually true?
I’m sure or at least hoping my UA levels would be below 388 since that’s what they were at 200mgs and now I’m taking 300mgs?
I’m worried this attack will never end and this pain is dissolving and crystallising again! I’m not sure what to do? Can it be an allergy? I was fine on 200mgs.
🙁

Will Epsom Salt Reduce Length of Gout Attack?
-
April 6, 2017 at 9:47 pm #3011
Patrick
ParticipantJames,
When I first started getting Gout Flares, they would last about a week because I didn’t know what they were nor how to treat them.
Let me ask you, have you tried Methylprednisone packs? It’s usually a 6 day pack that starts with 6 tablets the first day, then 5, then 4….and so on. If you haven’t used this antibiotic, I’d highly suggest you do. For me, I always keep an extra pack on me at all times, just in case. Usually, if I felt a Gout flare coming on, I’d hit it with the Prednisone and some colchicine and within 2 hours it was gone. But I’d make sure to finish the 6 day supply.
Try that. You can also get a steriod injection into the site which really helps also. Try the medication first. 12 days is way too long to be suffering brother.
-
April 6, 2017 at 11:15 pm #3012
nobody
ParticipantIn my mind, avoiding this situation is what colchicine is for. I never used (methyl)prednisone pills so for all I know that works as well or better. But the problem I had with NSAIDs is that they would bring welcome relief but not completely stop the attack or whatever it was.
If you count ‘the pain gets better some days and worse other days’ as one attack, then I’ve had attacks lasting a good bit more than 12 days, never knowning when I would be able to walk without crutches. And the time required for the joint to recover fully after that? Don’t get me started. I can’t prove it was gout but no one ever found another cause and it’s not because no one looked.
Colchicine may not provide immediate relief but my experience has been that if you take enough (which may be more than is recommended nowadays in your country) and wait, not only does the pain slowly go away but the joint goes on to recover fully within days.
Now this is only anectdotal evidence. Maybe I just happend to start using colchicine after I had already worked through enough of the underlying problem by improving my diet or something and that’s why my outcomes improved. Possibly NSAIDs were preventing natural healing and I only had to stop relying on them. What do I know?While prolonged use of NSAIDs is not recommended, what ‘prolonged’ means for you and for me might be very different things. If you’re still experiencing no side-effects after 10 days and a blood test doesn’t raise a red flag such as liver markers going crazy, I don’t see why you couldn’t use them longer. You’re probably addressing the underlying cause with allopurinol so it’s not like you’re going to make a habit of taking them every day.
I have abused NSAIDs in the past but the reason I say so is that there were warning signs. If you do not get any I would take that to mean you can handle the stuff. But I’m no doctor.As to UA tests, sure you can get one during an attack. The issue is: whatever for? Whether or not the result ends up being an outlier, it’s not going to inform your allopurinol dosage, is it? Whatever your doctor’s opinion about how skewed the data might be, would it be a good time to change your dose?
Extra data is always worth having of course. If you’re going to have blood drawn anyway, by all means get your UA checked while you’re at it. -
April 7, 2017 at 10:39 am #3014
d q
ParticipantHi guys, thank you both for such fantastic advice, just a few things I’d like your advice on;
@Patrick – tell me about it mate. It’s driving me insane. I’m just worried it’s the allopurinol causing this? I’ll definitely ask my doctor about Methylprednisone packs when I next see him. They sound helpful. Can a local GP do direct steroid injection? I’m based in the UK and the last attack I had she mentioned she can’t do a joint fluid test to confirm gout, Is it as difficult or tricky to perform? By the way Patrick, do you still get attacks whilst being on allopurinol?
@nobody – Thanks for your advice mate, I’m going to ask my gp for colchicine next week, I initially avoided it when it was offered to me at the start of my allopurinol treatment. Is it something I can use whilst in a attack or is it something I can only use when the feeling of an attack is coming? Also the blood form I have is only for urate levels so I don’t really want to use it if the results won’t be accurate? I mean is hit or miss with results or are tests generally completely wrong during an attack..? You also mention your attacks can last longer but are those long attacks you get part of the same chain of days or are they spread across weeks? My first and second attacks were over two weeks long! Lastly are you too taking allopurinol..?Thanks guys.
-
April 7, 2017 at 12:50 pm #3015
nobody
Participant“Is it something I can use whilst in a attack or is it something I can only use when the feeling of an attack is coming?”
Methylprednisone might be a better choice when dealing with a fully-developped attack.
The problem with taking colchicine whilst in a attack is that you might have to take more pills and that you likely won’t get quick relief anyway. So you ought to take it early but taking it late sure beats having an attack which doesn’t end.“You also mention your attacks can last longer but are those long attacks you get part of the same chain of days or are they spread across weeks?”
I haven’t had one of these for many years but they were like you said: “the pain gets better some days and worse other days”. To be clear: one joint affected by symptoms varying in severity but never completely going away.
-
-
April 7, 2017 at 3:09 pm #3016
d q
Participant@nobody “Sure beats an attack that doesn’t end”..? Now your worrying me! Are there actually attacks that go on for more then 3 weeks? This coming Sunday will mark two weeks of constant pain with varying degree. Any idea about urate test during an attack (numbers being wrong or not)? Are you taking allopurinol by the way..?
@Keith, any advice..?-
April 8, 2017 at 6:15 am #3019
nobody
ParticipantI think you have reason to hope that your attack will soon be over but yes, I’ve had symptoms lasting way too long. But after a while it becomes difficult to tell the ebb of such an attack from the symptoms that might only due to the damage it has caused, especially many years after the fact and without the help of notes. So I hope you’ll excuse me if I don’t give you a straightforward answer.
My experience hasn’t been that test results during an attack are all that strange compared to regular tests results. But then my test results have often varied quite a bit for no obvious reason.
For instance, between an test right at the onset of an attack and a followup test (less than 2 week afterwards), the reported value dropped by little more than 100 umol/l which is not much more than random drops I’ve seen over longer intervals (without the help of medication or major changes in weight or diet). I’ve also had a test done in the course of one of these long attacks actually coming back a good bit lower than a test done as I was recovering from it.
Again, the issue is: what would you do with a test result? If you’re going to compare it with the previous test to decide whether to discard it as an outlier or not, that’s not going to provide much new information and you might as well assume your UA is more or less the same as it was the last time you were tested.
I think the value of UA testing can easily be overrated and that most of the value lies in robust trends, not in single tests.Finally, I am not taking allopurinol.
But you may nevertheless be interested to know that I’ve never had one of these single-joint unending attacks since I lowered my median UA test under 400 umol/l. You lowered your UA quite a bit more brutally than I did which is probably best in the long run but I guess increases your risk of experiencing a serious attack, at least if that brutal drop doesn’t also bring your UA well into the safe zone under 300.
-
-
April 7, 2017 at 4:06 pm #3017
Patrick
Participant@Patrick – tell me about it mate. It’s driving me insane. I’m just worried it’s the allopurinol causing this? I’ll definitely ask my doctor about Methylprednisone packs when I next see him. They sound helpful. Can a local GP do direct steroid injection? I’m based in the UK and the last attack I had she mentioned she can’t do a joint fluid test to confirm gout, Is it as difficult or tricky to perform? By the way Patrick, do you still get attacks whilst being on allopurinol?
James,
I’m not sure about a GP doing a steroid injection. I’ve always had my Rhuemotologist do it, or his assistant do it. It’s actually a Prednisone injection right into the area where the pain is. For instance, my trouble spot was my left ankle. If I couldn’t control the pain within a few hours, I’d head over to my Rheumotologist and he would give me the steroid injection and within an hour or two, the pain was gone completely. Now I’m sure you understand that this was just strictly for the pain, not the actual cause. You are already dealing with the cause, as you’ve stated.
I’ve been lucky. Since I’ve been on Allopurinol (over 18 months now), I’ve had one Gout Flare, last June. I felt it coming, immediately took Colchicine and 4 Methylprednisone tablets and within 2 hours, it was gone. I then continued the steroid pack the rest of the week, supplemented a few Naproxen in there for good measure, and haven’t had an episode since. Nor have I had any lingering pain. Occasionally, I DO get tingling in my big toe, but nothing like a major flare up, and usually I can kill that with 600-800 mgs of Naproxen.
I hope that helps, brother. No one should be living with this pain for as long as you have. Keep us posted.
-
April 8, 2017 at 11:51 pm #3021
d q
Participant@nobody, interesting information there mate, thanks. I really do think this was all due to the increase in allopurinol. My UA levels were 388 just over a month ago when on 200mgs and literally 5 days after starting 300mgs the attack hit. I’m guessing the UA levels must have dropped pretty low after hitting 300mgs which probably caused the attack.
@Patrick, thanks man. I’ll check with my GP next week both about the injection and Colchine and see what they advise going forward whilst the allopurinol does its thing. With regards to naproxen do you take 500mgs twice a day when you get that feeling? And how long for? On another note, have you ever had an attack follow another attack in the same place prior to starting or just after starting Allopurionol..? Thanks pal.
Epsom Salts For Gout
On a general note, whilst dealing with this pain I decided to do some intense googling about relief techniques and came across using Epsom salt and dissolving it in warm water and placing your foot in for a foot soak. Now I know many people will say it may just be psychological or just coincidence but my foot really does feel much better. The inflammation also seems to have come down. Was it the salt or was it the warm water, who knows.. But there seems to be some link to Epsom salt and uric acid. Ultimately what matters is the end result and we’ll see how I feel tomorrow.
@Keith, any advice on length and severity of an attack outside of using any pain relief or anti inflammatories and just allowing the body to deal with the inflammation alone (taking allopurinol only)? Thanks-
April 12, 2017 at 3:12 am #3133
 Keith TaylorParticipant
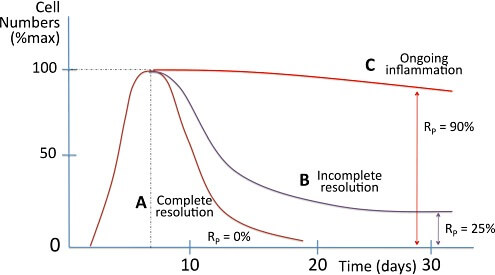
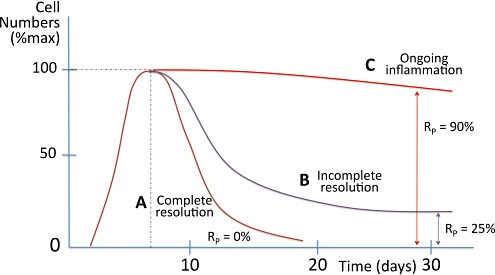
Keith TaylorParticipant@d-q if we could isolate a single gout attack, I’d say 5 to 7 days to resolve it naturally. Also, I’ve recently learned a little bit about how we might reduce that to 3-5 days. Because what we eat can influence how quickly inflammation subsides. So, as we learn more about efferocytosis, I’ll probably get a better idea of numbers of days for natural gout flare resolution. In any case, it’s good to be aware of factors we can manage to avoid lingering gout.
But, if you don’t get uric acid below 300μmol/L (or at least below 350, i.e. 6mg/dL), you are likely to get another attack. Which is likely to happen before the previous one resolves. Therefore, the Gout Hell scenario that I mentioned earlier seems relevant now.
So that’s why a good plan is essential. Because you need to get through the Gout Hell risk zone as quickly as possible. Also, nothing I’ve read recently persuades me that my personal plan is wrong.
Firstly I learned to control gout pain so I could stop an attack within half a day. Usually, around 2 hours, max.
Secondly, I safely titrated allopurinol up to the max. Which is 900mg per day in the UK, 800 in the USA.
Also, that allowed me to do 2½ years on allopurinol. Then, 3¼ years without meds (but I think I’m pushing it now!).In conclusion, I guess I just like to get on with it. Because I spend far too much time procrastinating before I act. Maybe, other people like to start quicker. Then, edge forward at a slower pace.
-
April 12, 2017 at 12:52 pm #3158
nobody
ParticipantAbout the hot water thing: http://goutpal.net/forums/topic/first-gou-attack/#post-3157
-
-
April 14, 2017 at 12:09 am #3167
d q
Participant@Keith, good to hear from you mate. I wish my attacks lasted 5-7 days. This Sunday will make this attack 3 weeks. Its much much better now though and I can walk on it albeit painfully. A mistake I made may have been stopping Naproxen 10 days into treatment because I felt it was doing nothing for me (it brought very slight pain relief and I couldn’t see much in the way of inflammation reduction). I was taking the maximum prescribed dose of 500mg twice a day. I’m getting my UA levels tested on Monday and was hoping you could advise if these results would be accurate whilst being at the end of an attack or if I should delay the blood test till later..?
@nobody, yep read that post, thanks. I can guarantee you that soaking my the affected foot in Epsom salt really did work. It definitely brought me relief.
Take a look at this site which also has input from Keith: -
April 14, 2017 at 8:30 am #3180
 Keith TaylorParticipant
Keith TaylorParticipantI would get the uric acid test irrespective of the timing of gout attacks. Because, I don’t think it will make any significant difference to your treatment plan. For example, if your level was temporarily reduced from 380 to 370μmol/L, you’d still to increase allopurinol dose.
On the other hand, if your results showed a surprisingly low figure, you could easily arrange a follow-up test in two weeks. So, overall, from memory of your uric acid test results, I think the sooner you get uric acid lower, the better. Because, it seems to me that your current level is causing the dreaded Gout Hell. That is, repeated gout flares as old crystals start dissolving, then re-form.
-
April 14, 2017 at 2:01 pm #3182
d q
ParticipantHi Keith, I think it’s gout hell too. It’s partly my fault for trying to walk on it too soon. I should have potentially gave it another few days or so. All of that healing seems to have gone to waste. I’ll get them done tomorrow while I can still walk. I feel it might be my last chance!
Just out of interest;
did you titrate on your doctors advice or just because you did your own research?
Also what did you get your uric acid levels down to whilst being on 900mgs for those years?
Did you suffer any side effects?
Finally suffer an attack after attack on 900mgs for a few months?Thanks Keith, you’ve been fantastic in helping me.
-
April 14, 2017 at 8:05 pm #3186
 Keith TaylorParticipant
Keith TaylorParticipantIn my experience, walking gives faster gout flare recovery. So, I believe you are just getting repeated attacks because your uric acid level is in a bad place. But, your next uric acid test results will provide better information.
“did you titrate on your doctor’s advice or just because you did your own research?”
A mixture of doctors advice and my determination. Because 3 doctors were happy to stop titrating once I reached average. But, I like to think I’m better than average. Then my fourth doctor was very supportive. So once I’d got to 300mg/day with no ill effects, I rapidly went to 600, then 900mg allopurinol per day. The doctor prescribed colchicine to take for 2 weeks at dose change. But, on the whole, I relied on max strength ibuprofen and paracetamol.“Also what did you get your uric acid levels down to whilst being on 900mgs for those years?”
I recall it was less than 300μmol/L. But, I can’t remember the exact figure. So, I’m going to try and get my history when I see my doctor after Easter.“Did you suffer any side effects?”
No“Finally suffer an attack after attack on 900mgs for a few months?”
No, attacks were very rare, and I was prepared for them. I feel all my preparation was worthwhile. Because I knew exactly what to ask my doctors. Also, I knew that my best chance of least-pain recovery was to get as low as possible, as fast as possible.“Thanks, Keith, you’ve been fantastic in helping me.”
I think you’ve helped me more! Because I cannot run this forum unless people like you are brave enough to discuss their health in public. So, you should be proud d_q! Because thousands of silent readers benefit from your questions and our discussions.
-
-
April 19, 2017 at 11:24 am #3337
d q
ParticipantHi Keith,
Just a few updates, With a lot of effort I finally managed to get myself to the hospital to do that blood test. Results are as follows:
Kidney function is fine, liver function is fine, uric acid has dropped from 388 to 336 as a result of moving up from 200mgs to 300mgs of allopurinol. I also saw my GP and explained that I’m in the middle of an attack that’s been going on for nearly 4 weeks and if I should move up to 400mgs per day. She agreed and said go for it. She also gave me a prescription for naproxen and said start that alongside your allopurinol increase to preempt any possibility of an attack.I wanted your advice on if I should go for the 400mgs or if I should wait until I come out of this attack (If I ever do)..?
Or should I remain on the 300mgs of allopurinol and at a uric acid level of 336 and let debulking occur at a slower rate?
Finally, or should I wait longer and do another test after a week or so to see what the result would be then as it may actually be lower then 336?
(Baring in mind the 336 uric acid result is while I am in the middle of an attack)
Thanks as always mate.
-
April 24, 2017 at 12:49 pm #3352
 Keith TaylorParticipant
Keith TaylorParticipantI’d always aim lower as quickly as possible. But, I’m happy that your latest question has once again set me off on new research. Actually, it’s updates from Start Allopurinol Quickly, But Carefully, which I mentioned in my recent Gout Gamechangers post. More researchers have agreed that waiting for gout flares to resolve is not usually good for uric acid control. But, they also emphasize the need to manage on a case-by-case basis. So, basically, it’s up to you.
However, I’d like to share my logic. Because, I believe there are benefits from getting well below 300μmol/l uric acid. To explain, the risk comes from partially dissolved crystals. So, if uric acid in the blood is lower, that reduces the time that crystals are partially dissolved. Therefore, it reduces the risk of flares occurring from debulking.
Finally, I’ve often stated there is no lower limit. However the latest guidelines from European rheumatologists suggest that we shouldn’t maintain uric acid below 3mg/dL for long periods. Because, there is some evidence to suggest that:
uric acid might protect against various neurodegenerative diseases such as Parkinson’s disease, Alzheimer’s disease or amyotrophic lateral sclerosis
Of course, that doesn’t mean that we should not consider very low levels to speed the debulking process. But, we have to weigh up all the personal aspects of each individual case. Unfortunately, it’s hard to find doctors who have the time to explain every last detail.
-
April 29, 2017 at 10:36 am #3440
d q
ParticipantHi Keith, I read that article and the logic makes perfect sense to me too, thanks. So I’ve decided to go ahead with the 400mgs dose. I’ve started off slightly slower by taking 400mgs on alternate days for a week and will go the full 400mgs starting Monday.
I’d also like to mention that my attack has finally substantially subsided. The inflammation has almost completely gone and I’m able to walk on it far more frequently. There is still discomfort there but I think that’s just the muscles in the foot adjusting to being able to walk on it correctly flat again (I hope anyway).
The quicker recovery “seems” to have come from the hot foot soaks in Epsom salt and the “possibility” of the increase of allopurinol to 400mgs on alternative days a week ago. That’s inconclusive though but it could be further proof of your article and research.
Once the attack completely subsides I’ll take another blood test to check UA levels on 400mgs daily and update you. I’m also expecting an appointment letter from a new rheumatologist as I’m not comfortable with my existing one due to he’s explanations and treatment plan.
Finally mate, I was wondering how long you too the maximum dose of 900mgs allopurinol and if you managed to check those UA levels for me as I really want to discuss with my rheumatologist if I can do the same and then take time off allopurinol like you?
Thanks for everything Keith, you’ve been so supportive.
-
April 29, 2017 at 11:55 am #3441
nobody
ParticipantEven muscles can take a while to heal and de-atrophy.
Low blood UA + blood flow ought to dissolve crystals.
But be aware that as your crystals have evidently already been dissolving, your blood UA has only one way to go as you get rid of them: down. Unless you’re going back to alcohol or something, your equilibrium UA on your current dose ought to be a good bit lower than anything you’ve experienced so far.
Even if you haven’t experienced side effects and your blood tests show no stress, the higher your dose, the more chances you’re taking. So don’t overdo it, especially if from now on you only get pain that goes away on its own within a few hours to a day. -
April 4, 2020 at 9:56 pm #9284
 Keith TaylorParticipant
Keith TaylorParticipantPeople have been asking about Epsom Salts for gout recently. Among other things we found:
- There was a variety of experiences ranging from “Epsom salt soaks make my gout flares less painful” to “never works for me so I stick with pain meds”.
- One person contributed a quote from an arthritis study:
The results of the study concluded that foot bath with Epsom salt procedure was effective in reduction of joint pain, stiffness and improving the … disease such as osteoarthritis, gout, rheumatoid arthritis and juvenile rheumatoid arthritis
Sabitha, M. “Evaluate the effectiveness of hot foot bath with Epsom salt on joint pain, stiffness, and physical function among patients with osteoarthritis in selected hospitals at Ottanchathiram.” PhD diss., Bishop’s College of Nursing, Dharapuram, 2018.
But if anyone else wants to discuss Epsom Salts for gout, it’s probably better to start a new topic.
-
-
April 30, 2017 at 8:47 pm #3478
d q
ParticipantThanks for your encouraging words nobody. Yes, I’ve noticed my muscles are definitely not taking too kindly walking the correct way and not on the outer side. I’m hoping that would subside in a few days.
The 336 ummol measurement was taken during the gout attack so I’m not entirely sure just how accurate the reading will be when everything clears up eventually but I’m definitely trying to keep the blood flowing to that area as much as possible and to be honest am hoping that 300mgs is enough. I started the 400mgs to clear things out quicker and because I believe I was in gout hell. Once the attack subsides I’ll be sure to check my levels again and see if 300mgs was all in fact that I required but for now I think 400mgs is my best bet, if it’s significantly lower then maybe I can revert back to 300mgs again. I’m not really an alcohol drinker and might have the occasional beer once every month but nothing really more. Believe me mate, I’m trying my best to find my optimum lowest medication dose as quick as possible as gout is seriously debilitating and I just don’t want anymore attacks. This flare up was two back-to-back and was a disaster. 5 weeks.
I’m also waiting on Keith’s response is on my previous post as I’m thinking of doing the same thing (maximum dose for a period of time to flush out and do a major debulk then taking time off allopurinol or at least taking a very low maintenance dose afterwards).
I’m not too sure what you mean by if I start getting pain that goes away within a few hours to a day? Would that be for a limited time because of final crystals dissolving?
p.s. Do you have a nickname we can use, thanking nobody is a little strange 🙂
-
April 30, 2017 at 10:22 pm #3479
nobody
ParticipantWhat I meant was: if you stop getting long-lasting pain.
I don’t know that you can tell how much solid UA is left based on symptoms. But my thinking is that the average pain duration is an indicator of where your blood UA is at relative to your needs. Even if blood tests were perfectly reliable, the amount of UA in your blood is only part of the story of crystallization.
I understand increasing your dose is tempting but I’d make sure it serves a useful purpose before taking chances. At some point you’d experience diminishing returns anyway. I don’t know if that’s where you are already but I would certainly stop taking a larger dose than necessary once I felt safe from long-lasting pain. And the faster you’ve increased your dose, the quicker the dose required for you to feel safe ought to diminish.
That said, I wouldn’t drop my dose as soon as pain subsides. Think weeks, not days.The strangeness involved in calling myself Nobody is deliberate. If you don’t like strangeness, you could use Tawrikt for instance.
-
-
May 1, 2017 at 12:20 pm #3483
d q
ParticipantHi Tawrikit 🙂
At some point you’d experience diminishing returns anyway.
Unless I understand wrong, do you mean damage to health from allopurinol then any more useful gain from it..?
And the faster you’ve increased your dose, the quicker the dose required for you to feel safe ought to diminish.
I’m not too sure why that makes sense, the speedier increase generally assists in debulking quicker so if anything allows to get on and off the dissolve train quicker? That’s as far as I’ve been understanding it so far. Providing no health problems are sought in the first 100-300mgs trail of allopurinol
That said, I wouldn’t drop my dose as soon as pain subsides. Think weeks, not days.
This is why I was thinking of hitting 400mgs for a month or so until this attack has fully healed +- another 2 weeks or so extra for safety (I cannot believe it has taken this long) and to check levels again in a month time whilst on 400mgs and then possibly adjust from there back down to 300mgs to see if that dose is suitable going forward. I would assume that 300mgs is not really enough though because its so close to 350 ummol which is round about were gout hell starts and warning labels kick in. Unless 336 ummol was inaccurate because I was in the midst of an attack and it could actually be much lower.
This is why I was contemplating a heavy debulk with a relatively high dose for 6 months and then relaxing my dose right down or even stopping it for a little (I’m not a fan of medication either but its pain for gain).
I think that’s the approach Keith has taken.-
May 1, 2017 at 1:33 pm #3484
nobody
ParticipantDiminishing returns: there are limits to how fast this ‘debulking’ can happen. It’s not only about how much UA you have in your blood.
The main point of getting your UA lower than it needs to be is to make your flareups shorter and less severe.UA blood tests: you haven’t done enough tests to get a decent picture of what’s going on but to the extent you are ‘debulking’, all tests will be biased high. If you’re already taking more than you need to (obviously I can’t know whether that is indeed the case), your test results will trend down even if you do not increase the dose further.
-
-
May 2, 2017 at 7:39 pm #3491
d q
ParticipantAgreed, but I won’t be able to tell if 300mgs or 400mgs is the dose that’s required until I come out of this so far 5 week attack. I mean don’t get me wrong I am able to walk around but I put on my asics today to have an extended walk around the area and now my ankle and the surrounding muscles hurt. The ball of my foot also hurts a little and now it’s got me worried another attack is following. I guess we’ll find out in a few hours. Unfortunately I can’t take colchicine so took 400mgs of ibuprofen before hitting the 500mgs naproxen.
One thing I did notice was you mentioned Uric Acid only has one way to go: Down(3441) as crystals dissolve but a little further down you mentioned that your results will probably be biased high(3484) as crystals dissolve. I think the results would most probably be as your second post suggests (high) as they dissolve.Keith, I was wondering if you had a chance to take a look at my previous few posts and advise..? Specifically Reply #3440.
Thanks
-
May 2, 2017 at 8:33 pm #3492
nobody
ParticipantYes, if your test results are temporarily elevated that implies they are expected to go down in the future… two ways of saying the same thing.
Variations are to be expected but the average daily mass of dissolved crystals should diminish over time which is why you can expect your UA to trend downwards.I hope you’re experiencing pain from exercising injured and under-used muscles and tendons rather than arthritis.
But exercise might cause more crystal deposits to dissolve… which isn’t what you want right now because your system is apparently already struggling with the UA from deposits dissolving on their own. If too many crystals dissolve at the same time, you risk a serious attack.
Once you are mostly free of serious symptoms, you may want to speed up the dissolution of the remaining deposits with exercise. Until then, be careful.If you can’t take colchicine, what about oral methylprednisone or similar?
I assume you are aware that the side effects of ibuprofen and naproxen add up.
If this class of drug (NSAIDs) is the only thing you can take for symptoms, I guess that would warrant taking a bit more allopurinol initially than someone who is able to take any drug.I hope Keith will answer your questions because we do not always agree.
-
-
May 3, 2017 at 4:55 am #3493
 Keith TaylorParticipant
Keith TaylorParticipantnobody, I think it’s great that we bring different points of view to this forum. After all, gout management has to be tailored to each individual. Therefore different gout sufferers will, and should, make different choices.
Also, there are often several different ways to reach a solution. So, the only wrong way is that which is taken without considering patient needs. I realize this is a generalization. But, pain control is a good example. Personally, I think steroids are to be avoided at all costs. Yet, I vaguely recall an article by a rheumatologist. Where he explained that sometimes they can be the right choice. So, my approach generally is to look at what a gout sufferer is trying to achieve. Then, work from that, gathering relevant personal facts, to find acceptable, appropriate, gout therapies.
Unfortunately, I’ve completely lost the point of this topic. Also, it’s very long for finding any outstanding questions. So, d_q, can I ask you to start a new topic for any unresolved questions. In fact, unless they are closely related, I prefer one question per topic. I’m not trying to be awkward here. I just want it to be clear to other gout patients who are looking for information about general gout attack severity and gout duration.
-
May 5, 2017 at 10:21 pm #3588
d q
ParticipantHi Tawrikit,
I assume you are aware that the side effects of ibuprofen and naproxen add up. If this class of drug (NSAIDs) is the only thing you can take for symptoms, I guess that would warrant taking a bit more allopurinol initially than someone who is able to take any drug.
My pain tolerance level is generally very high and I hardly use any pills at all (aside of allopurinol). I only really take Naproxen if I feel an attack is coming and if it doesn’t bring relief within a week I stop it anyway. I then just take a tablet or two of Ibuprofen if I have complications sleeping or if I’m really in pain. Longest Ive taken Naproxen is for 10 days around 2 months ago and the time before that was 3 months ago for 3 days.
Yes, if your test results are temporarily elevated that implies they are expected to go down in the future… two ways of saying the same thing.
Variations are to be expected but the average daily mass of dissolved crystals should diminish over time which is why you can expect your UA to trend downwards.This is indeed encouraging, frankly speaking I am really hoping that is the case so I can move back down to possibly 300mgs (just the one tablet rather then two) and less drugs in the system.
I hope you’re experiencing pain from exercising injured and under-used muscles and tendons rather than arthritis.
But exercise might cause more crystal deposits to dissolve… which isn’t what you want right now because your system is apparently already struggling with the UA from deposits dissolving on their own. If too many crystals dissolve at the same time, you risk a serious attack.
Once you are mostly free of serious symptoms, you may want to speed up the dissolution of the remaining deposits with exercise. Until then, be careful.This is exactly my worry. The actual pain from my initial gout attack on my left toe has somewhat gone (minor inflammation is present but the majority of the pain has subsided). What has actually become very painful is the entire ankle/foot. All I did was put those asics on and go out for a 3km walk and all of a sudden this occurred. I can walk on it fine for short periods of time but it does get painful after a while. It seems as if crystals in the whole area are dissolving? Can that be the case? Or do you think this may be a side affect of increasing my allopurinol to 400mgs?
Keith, no worries mate. I’ll start a new topic with the questions I wanted to ask you in specific about how your dealt with your treatment plan.
-
May 7, 2017 at 12:37 pm #3622
nobody
ParticipantI’m replying here in order to leave the other thread unanswered.
You asked: “It seems as if crystals in the whole area are dissolving? Can that be the case? Or do you think this may be a side affect of increasing my allopurinol to 400mgs?”
I can’t know what’s going on in your body.
One can imagine several processes which could cause something like that to happen. You could conceivably for instance temporarily get UA re-crystallization following the dissolution of a large deposit. But allopurinol side effects wouldn’t be at the top of my list, unless of course by “side effect” you mean dormant UA deposits being disturbed.
I don’t see much point in overthinking this. If your symptoms are arthritis (I can’t tell based on a forum post) then time is on your side. You have lowered your blood UA and you knew this might temporarily trigger more frequent bout of arthritis. And in case you didn’t know, it might give you arthritis at the weirdest locations too. That is what curing gout feels like. Summon some patience, make sure your muscles aren’t tensed for long periods due to pain or posture (your salt baths ought to be good for this) and relax.
As I mentionned earlier, in my thinking you can assess the effectiveness of a UA-lowering intervention by looking at the average duration of your symptoms. If most of your symtoms go away quicker than they used to, you are on the right track no matter how unusual the symptoms are.
If on the other hand you think you might have something other than arthritis such as an infection (do you have a recent wound near the affected area?), consider seeing a doctor. -
May 15, 2017 at 5:46 am #3661
 Keith TaylorParticipant
Keith TaylorParticipantyou can assess the effectiveness of a UA-lowering intervention by looking at the average duration of your symptoms. If most of your symptoms go away quicker than they used to, you are on the right track no matter how unusual the symptoms are.
That’s a great reason for maintaining a gout diary. Because, as well as recording test results and treatment changes, you can also record symptoms. Especially, if you record days with no symptoms, you have good information to confirm gout recovery.
As humans, we tend to focus on the unusual, then forget all the good days when we are symptom-free.
-
-
February 28, 2019 at 6:16 am #8830
 [email protected]Participant
[email protected]ParticipantGout Flare VS Gout Attack
How do you gauge the difference between the two? What’s your threshold considering pain and swelling as factors?
I’ve what I considered four full-blown attacks in my first four years of experience with this affliction, skipped two years, had a bad one last April, and one other not quite as bad a few months later. But I’ve been riddled with flares for the rest of the past nine months.
I’d say attacks entail significant swelling, with possible displacement of the joint, accompanied by excruciating amounts of pain. As they’ve always occurred in my foot, so mobility is severely affected and swelling will make putting a shoe on practically impossible. I thankfully have never had an attack severe enough where “the weight of a bedsheet” on my foot was painful.
Flares on the other hand, have been far less severe in both pain and swelling, varying from annoying or slightly uncomfortable, to moderate swelling with bearable pain, possibly strong enough to result in a limp, but not cause severe mobility issues.
So what’s your barometer for attack vs flare?
-
February 28, 2019 at 8:24 am #8831
nobody
ParticipantI don’t know that these words are defined anywhere in a standard manner. Some people might use these two words to mean the same thing.
Because of the different locations which might be affected, you could for instance have severe mobility issues or be unable to put your shoes on (not necessarily both at the same time) without much pain at rest. You might also not see much (if any) swelling or redness if the inflammation is deep under the skin.
So what we’ve got is mainly a standard description of the textbook MTP1 (big toe joint) attack: severe pain (at rest as well as to the touch), swelling (with unusually warm skin) and redness. But not having all the signs doesn’t mean it’s not gout, especially if a different location is affected. If you want to call it flare rather than attack when your big toe gets some but not all the symptoms or when the pain isn’t that bad, that makes sense but don’t expect everyone to use the word “flare” that way. -
February 28, 2019 at 7:50 pm #8832
 [email protected]Participant
[email protected]ParticipantI understand that “flares” aren’t a technical medical term, I literally meant “you” as in the members of the forum. I’m curious how other sufferers are gauging their own experiences. I saw the “Monitor Your Gout Pain” graph after I posted this, and I’d basically say levels 1-5 I’d call flares, and 6-10 I’d classify as an attack. The attack that started this ten month run was probably an 8 on that scale, and I’ve been bouncing between 0-4 regularly since, with a couple of forays into the 5-6 range.
My primary source of discomfort these days isn’t my big toe at all, it hasn’t bothered me in months. In fact, the big toe joint has flattened back to totally normal looking. For whatever reason, my crystal deposits have migrated one joint over to the base of my second toe. It sometimes looks like I have a little marble in what you’d call the Proximal Phalanx. It’s looked slightly puffy for months, and it swells a bit more roundly when I “flare”.
-
February 28, 2019 at 9:07 pm #8835
nobody
ParticipantAs you can see the forum isn’t very active and so the members of the forum pretty much all use words in their own way.
I’d say the duration, location and specificity of the symptoms matter as much as the pain. The main thing I take away from your description for instance is that you’d probably benefit from increasing your allopurinol dose sooner rather than later (assuming the blood test doesn’t come back with a red flag). And that’s got nothing to do with pain levels. Instead, I focused on things like “slightly puffy for months” because one of the points of increasing one’s dose slowly is to avoid triggering inflammation. But it looks like you might have constant inflammation to begin with! Inflammation in a single location which hasn’t resolved after a week also suggests you might have too much uric acid in your blood.
Either you take the time to describe your symptoms or you don’t. If you want to sum them up with a word or two, I don’t think the choice of word matters a great deal: absent a fairly detailed description, people will have trouble guessing what’s happening to you.
Gout symptoms vary quite a bit, which is part of why doctors have so much trouble diagnosing gout when you’re not in the middle of a textook acute MTP1 episode. Indeed I wouldn’t swear the ongoing symtpoms you’re experiencing on your second toe joint are due to gout. Don’t get me wrong: it’s probably gout. But if you didn’t have big toe attacks for several years previously, I would be more skeptical.In all likelyhood, you had deposits there for years by the way (they haven’t migrated).
It’s your body’s irritation with the deposits which migrates, for instance because some dormant deposit becomes unstable or because fresh crystals develop next to it. -
March 1, 2019 at 5:35 am #8838
 [email protected]Participant
[email protected]ParticipantExcellent advice as always, thank you. That second toe joint has been flaring regularly for a while now as I said, every week or two for a few months. I assumed it stays puffy because it hasn’t gotten a break, pointing to as you said, consistently elevated UA levels, not having a chance to shrink down enough before the next flare puffs it again. It was just about normal looking when I had a flare the second week after I started the Allopurinol, and it twinged a little two days ago.
I had the blood test done today, so I should have results by the middle of next week. Then my doctor and I will discuss what to do about dosage based on initial results. And of course I’ll report everything here, and ask what the opinion is.
-
-
AuthorPosts
The forum ‘Help My Gout! The Gout Forum’ is closed to new topics and replies.